NWAS Quality Account 2024-25 (1MB pdf)
Quality Account 2024/25 feedbackOn this page
- Chief executive statement
- Statement of directors’ responsibilities in respect of the Quality Account
- This year in brief 24/25
- About us
- Our shared purpose, vision and values
- Our strategy
- Our services
- Our Quality Strategy (23/26)
- Our aims and achievements in 24/25
- Our operational performance
- Our quality assurance
- Our improvements
- Quality aims 25/26
- Formal statements on quality
- Stakeholder feedback
- Appendices
- Research publications 24/25
- Contact details
Chief executive statement
Although I have been with NWAS for many years, this is the first Quality Account I present to you as Chief Executive and I am delighted to be able to introduce a publication which contains the many positives achieved during the last year.
The purpose of this report is to outline the progress we’ve made in improving the quality of care we provide for the North West region and sets out our priorities for 25/26.
At North West Ambulance Service NHS Trust (NWAS), patient care underpins everything we do. In most cases, people call us when they are at their most vulnerable – this is something we are acutely aware of, and it is a privilege to be there for them when they need us most. We remain committed to delivering safe, high-quality, responsive care for all.
The past year has brought continued challenges across the NHS, including changing demand across the four Integrated Care Boards (ICBs) we serve and ongoing hospital handover delays. Despite this, we’ve made strong progress particularly in our emergency call handling and response performance.
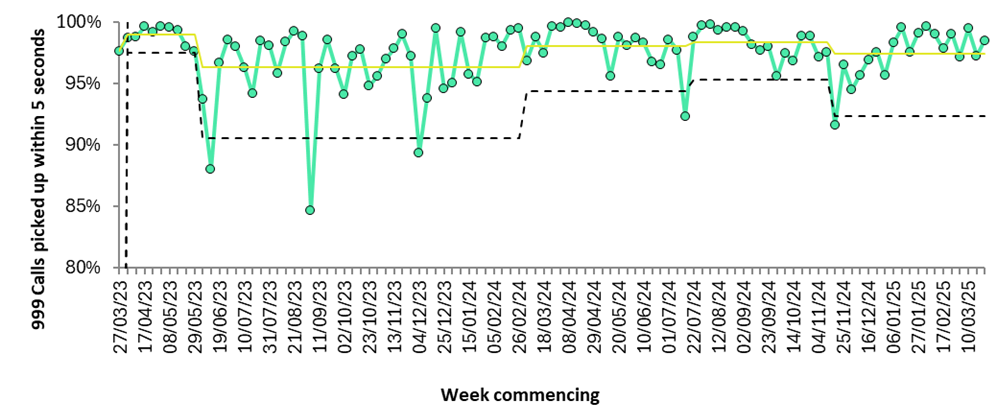
In 24/25, NWAS ended the year with a 999-call pick-up mean time of just one second, consistently ranking us among the top two ambulance trusts in England. Rapid call answering is a critical patient safety measure, especially for life-threatening Category 1 calls where early cardiopulmonary resuscitation advice can be lifesaving. We answered 97.8% of 999 calls within five seconds, maintaining one of the best performance records nationally.
Our response to Category 1 calls, the most urgent, has improved and continues to show sustained progress. Encouragingly, response times for lower acuity Category 3 and 4 calls have also improved for the second year in a row, now reaching levels not seen since before the pandemic. While prioritising the most urgent calls is essential, we remain focused on improving the experience of all patients.
We’ve strengthened partnerships with health and care providers to reduce hospital attendance and support care closer to home. This helps ensure ambulances are available more quickly for other patients. By addressing more cases via telephone, emergency ambulances are prioritised for patients in more urgent need.
Hospital handovers remain a key challenge, affecting ambulance availability. While some areas of the ICBs have seen improvement, others continue to face delays. We’re actively working with system partners to reduce these pressures and improve patient flow, ensuring that our crews can be available to respond more quickly and safely.
In 24/25, 85% of calls to 111, were answered within 60 seconds, this represents a 33% improvement from the previous year and the call abandonment rate reduced to 2.7%, a 10% drop. We also made significant strides in integrating our 999, NHS 111, and patient transport services (PTS) into a single, more efficient contact centre. Phases 1 and 2 were completed during the year, and Phase 3 was approved in January 2025. We’re now mobilising the final stage to embed the integrated contact centre model in 25/26.
Cultural transformation continues to be a strategic focus. In 24/25, we launched the North West Improvement Academy to build improvement capability from board to frontline. The first cohort completed nine months of training supported by internal and external experts. This forms part of broader efforts in organisational culture, workforce, and wellbeing, as detailed in our Annual Report and supporting documents.
None of our progress would be possible without the dedication of our people. I am constantly inspired by the commitment, compassion, and resilience of our staff and volunteers. Their contribution to the health and wellbeing of the North West cannot be overstated and I am extremely proud of the care they provide from both a clinical and emotional perspective. A kind word, reassuring advice and empathy can go a long way in easing an individual’s distress when they are scared, worried or unwell.
This Quality Account reflects the improvement, innovation, and care delivered every day at NWAS. Whether you’re considering joining our team, collaborating with us, partnering with us, or simply learning more about what we do, I hope this report gives you a clear sense of our direction and purpose. We are more than blue lights, we are a vital part of the region’s urgent and emergency care system, striving every day to make the North West proud.
Salman Desai KAM
Chief Executive
Statement of directors’ responsibilities in respect of the Quality Account
Under the Health Act 2009, National Health Service (Quality Account) Regulations 2010 and National Health Service (Quality Account) Amendment Regulation 2011, the directors must prepare quality accounts for each financial year. The Department of Health has issued guidance on the form and content of annual quality accounts (which incorporate the above legal requirements). In preparing the Quality Account, directors must take steps to satisfy themselves that:
- The Quality Account presents a balanced picture of our performance over the period covered.
- The performance information reported in the Quality Account is reliable and accurate.
- There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice.
- The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review, and the Quality Account has been prepared in accordance with Department of Health guidance.
The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account.
By order of the Board
This year in brief 24/25
Our services
| 999 calls we answered | 1,436,333 |
| NHS 111 calls we answered | 1,870,669 |
| Patient transport service journeys | 1,458,446 |
| Emergency incidents requiring a response | 1,118,433 |
| Hear and Treat | 15% |
| See and Treat | 28% |
Ambulance response times
| Category 1 response time mean | 00:07:44 |
| Category 1 response time 90th percentile | 00:13:11 |
| Category 2 response time mean | 00:29:49 |
| Category 2 response time 90th percentile | 01:00:33 |
| Category 3 response time mean | 01:57:46 |
| Category 3 response time 90th percentile | 04:19:49 |
| Category 4 response 90th percentile | 04:32:33 |
Patient experience
| The number of complaints we received | 2,277 |
| The number of compliments we received | 1,150 |
| The number of Friends and Family Test we received | 22,394 |
| Dignity, compassion and respectful care | 92.8% |
Clinical effectiveness
| Cardiac arrest survival at 30 days (Apr – Nov 24/25) | 10.8% |
| Stroke care bundles delivered | 90.7% |
| Patients achieved a return of spontaneous circulation (ROSC) | 32.7% |
Patient safety events
| The number of patient safety events | 8,479 |
| Patient safety events resulting in no physical harm | 6,835 |
| Patient safety events resulting in moderate physical harm | 186 |
| Patient safety events resulting in fatal physical harm | 93 |
Successes and achievements
- Appointment of a new Chief Executive Officer.
- East Lancashire care home engagement project, reducing conveyance from care homes to hospital.
- Smart programme boosted by funding from NHS England.
- Further development of the electronic patient record (EPR).
- Awarded the Outstanding Service award for a joint training collaborative with midwives at Liverpool Women’s NHS Foundation Trust.
- Implementation of the NHS 111 ‘Option 2’ for patients who present with a mental health crisis.
- Rolled out Project 365 to support efficient ways of working and enable effective record management.
- Seven cohorts attended the Improvement Academy working on real time improvement projects.
- Patient Transport Service (PTS) have trialled an electric vehicle, receiving positive patient feedback.
- Sixty volunteers recruited with plans to recruit seventy more.
- Phase one and two of service delivery model review completed.
- Extensive patient engagement programme, utilising virtual, face-to-face and digital methods of engagement.
About us
North West Ambulance Service (NWAS) is one of the largest ambulance trusts in England. We provide services to over seven million people across a geographical area of approximately 5,400 square miles. We employ 7,757 staff from over 100 sites and provide services to patients in rural and urban communities, coastal resorts, affluent areas and in some of the most deprived areas in the country. We also provide services to a significant transient population of tourists, students and commuters.
The North West region is one of England’s most culturally diverse areas, with over 50 languages spoken by community members. Consequently, we place considerable emphasis on equality and diversity and public engagement activities to ensure that our services are accessible to all members of the community. There are more people living with long-term health conditions and, as people get older, we can expect there will be more people in our communities living with illnesses. We know from our data that the overall health of our region’s population has an impact on demand for our services.
A strategic focus is to collaborate with our integrated care systems (ICS) and integrated care boards (ICB) to support the delivery of public and population health agendas and urgent and emergency care services. We are the only regional NHS organisation in the North West that operates across five ICSs:
- Lancashire & South Cumbria Health & Care Partnership
- Cheshire & Merseyside Health & Care Partnership
- Greater Manchester Health & Social Care Partnership
- North East & North Cumbria ICS
- Joined Up Care Derbyshire (which includes Glossop)
Our shared purpose, vision and values
At NWAS our vision is ‘to deliver the right care, at the right time, in the right place; every time.’
Our shared purpose is to help people when they need us most. Based on this purpose, our strategy sets out our vision to deliver:
- Right care means that we will provide outstanding care that is safe, effective and focused on the needs of the patient.
- Right time means that we will achieve all operational performance standards for our paramedic emergency service, NHS 111 and patient transport service.
- Right place means that we will provide care in the most appropriate setting for each patient’s needs, taking fewer people to emergency departments by providing safe care closer to home, or referring people to other health and care pathways.
- Every time means that we will provide services which are consistent, reliable and sustainable.
To deliver our vision, our values of ‘working together’; ‘being at our best’ and ‘making a difference’ underpin all that we do. These values describe the ‘how’ and set the expectations for staff to provide compassionate care and improve outcomes and experience for our people, patients, and communities.
We provide high-quality emergency care to save lives and make a difference to people with life threatening illnesses or injuries. For those with less serious conditions, we will tailor our response to each person’s needs. This may include urgent clinical assessment, advice over the phone, referring them elsewhere or alternative transport for scheduled appointments.
Our strategy
We have three strategic ambitions:
- Provide high-quality, inclusive care
- Be a brilliant place to work
- Work together to shape a better future
At the end of 2024, we agreed to extend the current trust strategy by one year whilst work was undertaken to develop the new trust strategy and supporting strategies during 25/26. This will enable us to ensure both internal and external factors are considered, including changes in trust leadership structures and outcomes from the NHS ten-year plan. We aim to launch the new suite of strategies in March 2026.
Our services
Integrated Contact Centres (ICC)
Following internal reconfiguration of services, the ICC includes 999, NHS 111 and patient transport service (PTS).
999
Emergency operation centres (EOC) receive and triage 999 calls from members of the public as well as other emergency services. EOC staff provide advice and dispatch an ambulance service to the scene as appropriate. The clinical hub (CHUB) based within the EOC, assesses patients via telephone and provides the most appropriate care based on that assessment. This may be an ambulance (either emergency or urgent care), GP referral, referral to other services or self-care.
NHS 111
NHS 111 deliver services for the North West region and are major contributors to the delivery of integrated urgent care. We signpost patients to the most appropriate care highlighted to them following triage and informed by the Directory of Services.
Patient Transport Service
Patient Transport Services (PTS) provide essential transport to non-emergency patients in Cumbria, Lancashire, Merseyside, and Greater Manchester, who are unable to make their own way to or from hospitals, outpatient clinics or other treatment centres.
Paramedic emergency services
Paramedic emergency service (PES) services are delivered by solo responders, double crewed ambulances and approved private providers who together deliver 999 emergency care for the population of the North West.
Resilience
Our hazardous area response team (HART) and resilience teams are specially trained and equipped paramedics who provide a response to high-risk and complex emergency situations, including major incidents. They respond to major incidents to deliver our statutory responsibilities as a Category 1 responder under the Civil Contingencies Act 2004.
Volunteering
We have one of the largest and longest-established community first responder (CFR) schemes in England, with CFRs operating across all areas of the North West, providing an effective, complementary service in their local communities.
We also offer several other volunteering roles, including Patient and Public Panel (PPP), Voluntary Car Drivers (VCD), Voluntary Car Service (VCS), Welfare Support Volunteers and Vehicle Movement Volunteers.
Corporate services
As well as providing clinical services to patients, we provide a wide array of specialist, non-clinical corporate services. These wider teams offer a unique variety of services, for example, estates and facilities, communications, risk management, digital, vehicle maintenance, finance, and human resources.
Our Quality Strategy (23/26)
Our Quality Strategy 23/26 is one of four key supporting strategies that define our priorities over the coming years, enabling us to achieve our goals and realise our vision.
As the ambulance service for the North West, we are privileged to support people during some of the most critical moments in their lives. We save lives, prevent harm, and provide services designed to deliver outstanding outcomes. Every day, our teams go above and beyond to meet these expectations. We are incredibly proud of our staff, volunteers, leadership teams, and partners who all contribute to the care we provide.
Our Quality Strategy to 2026, continues to support the significant changes we have experienced and continue to navigate across our senior executive team, including the appointment of a new Chief Executive. We will continue to embed strong leadership, support continuity, and ensure that our quality ambitions are fully realised and aligned with the evolving direction of the organisation.
In shaping this strategy, we consulted with over 200 colleagues across the trust including leaders, frontline teams, and a diverse range of stakeholders and networks. This strategy is not just a statement of intent, it is a living, evolving document that reflects the voices of both those who use our services and those who deliver them.
We’ve taken substantial steps to understand how patients experience our care. We’ve listened to staff who raise concerns about patient safety, analysed incident reports, participated in staff forums, and carried out clinical audits, all of which have given us deep insights into the safety, reliability, and sustainability of our services.
Continuous learning remains central to our approach. We are committed to improving safety, effectiveness, and the overall patient experience. Our Quality Strategy is closely aligned with the overarching Trust Strategy and interwoven with our broader set of supporting strategies and plans.
We will continue to nurture a positive safety culture, strengthen our partnerships with patients and families, and embed the Patient Safety Incident Response Framework (PSIRF). Our learning, both from successes and challenges will inform strategic priorities, guide organisational focus, and be supported by our improvement, project, and transformation teams.
The strategy is grounded in current policy and evidence from improvement and implementation science, reinforcing our goal to become better every day. It brings together expertise from across the organisation to deliver shared quality goals through collaborative action, measurable outcomes, and strong governance.
This strategy represents our ongoing commitment to challenge ourselves, to learn, and to improve continuously. The opportunity for partnership working has never been greater, particularly with the establishment of primary care networks, provider collaboratives, and integrated care boards. We are committed to working more closely than ever with primary care, community, mental health, and urgent and emergency care providers to build truly integrated care.
We are proud to serve the people of the North West and our Quality Strategy reflects our unwavering dedication to improving care and delivering the highest standards for our patients and communities.
Our aims and achievements in 24/25
In last year’s quality account, we laid out our aims for 24/25. The paragraphs below outline our progress against these over the last year with the bold text outlining our specific commitments.
Safer care
To be able to deliver safe care we need to protect our patients and our staff from avoidable harm. This requires understanding the complexities of the systems we work in, to be able to critically examine contributing factors of why errors occur so that we can reduce future risks. This can’t be done in isolation and requires developing a culture of safety first with our people, our partners and our patients.
- Complete our safety culture surveys and have action plans for the improvement.
In 23/24 we completed safety culture surveys across the trust, rolled out a patient safety training curriculum and implemented the Patient Safety Incident Response Framework (PSIRF). Work in this area has continued throughout 24/25 with a focus on launching our NWAS Improvement Academy to build improvement capability.
- Review our learning forums to include integrated patient safety learning (incidents, complaints, claims), learning from deaths, freedom to speak up and have themed improvement action plans based on local learning.
Area Learning Forums have been reviewed to include integrated patient safety learning and the development of improvement plans. There is good evidence that these forums are starting to use local data to change practice. The Regional Clinical Learning and Improvement Group (RCLIG) which brings together staff from each area recently refreshed its terms of reference to ensure that triangulated learning is being presented and feeding up to and from the area learning forums.
- Include the patient safety incident response framework (PSIRF) priorities in action plans and find the improvements that can be made locally.
24/25 has been the first year using the Patient Safety Incident Framework. This has required a change in the way we approach learning to ask why events took place in the manner they did, requiring an appreciative enquiry approach to identifying and solving problems. Improvement plans linked to PSIRF priorities are being developed, for example changes to call handling, mental health and medicines management. Further work to embed this approach to patient safety will continue in 25/26.
- Involve nominated leads in the regional clinical learning improvement group (RCLIG).
The introduction of the Regional Clinical Learning Improvement Group has provided a space to be able to critically discuss and identify areas for improvement, with work streams forming from those discussions. Clinical Leads from each sector now attend and the group provides additional support and advice for improvement ideas. One success has been the communication and sharing of good practice through the ‘Learning Loop’ publications which has seen staff interest grow with a further wish to be involved in learning using this approach.
- Ensure safeguarding needs are addressed within training needs analysis and explore digitalising our safeguarding process.
During 24/25, our Safeguarding team has worked with the Learning and Development team to align all new roles with the appropriate level of safeguarding training and trust-wide training compliance has been maintained throughout the year.
We make safeguarding referrals to 27 local authorities within the geographical footprint. Referrals are made electronically via our support centre in Carlisle to the appropriate local authority with 39,561 safeguarding and early referrals made in 24/25. The journey to digitalise the safeguarding process has commenced with early scoping of the process completed. Further work is still needed to move this initiative forward to enhance an already robust system.
Highly effective care
Highly effective care means supporting people to achieve good outcomes so they can maintain or achieve the best quality of life. To ensure this happens, care must be based on the best available evidence with staff who feel confident in their knowledge and skills to be able to deliver that care.
- Develop a plan and evaluate the national AACE Clinical Supervision Framework.
Following a period of multiprofessional consultation, development of the Clinical Supervision policy has been finished and is now ready for implementation, embedding and evaluation in 25/26.
- Complete a review of clinical triage tools, including the implementation of Category 2 segmentation.
We have implemented the national category 2 segmentation principles outlined by NHS England through amendments to its clinical flow and concerted recruitment into the Advanced Practitioner in Urgent and Emergency Care cohort. This has resulted in the management of over 500 category 2 incidents weekly without the need for an ambulance attendance. Furthermore, we have adopted a flexible approach to the management of category 2 validation, enabling us to prioritise category 2 incident management in proportion to the risk within the NWAS system.
- Improve see and treat (S&T) rates through local improvement plans, agreed trajectories, data review and the adoption of improvement methodologies.
Our Right Care Programme works with partners across the North West to improve access and outcomes for our patients. The initiatives in the programme are designed to shift activity away from conveying patients to emergency departments and towards alternative places of care, ‘see & treat’ and ‘hear & treat’. We have successfully embedded alternative pathways and improved ‘hear & treat’ within the cohorts we have been working with. The tests of change conducted within the programme have shown significant impacts of these alternative pathways however application has been to a limited cohort of patients. Further evaluation of the impact on clinical outcomes and overall performance measures is now needed.
- Finalise the mental health strategic plan, learning disability and autism annual objectives and dementia plan.
In 24/25 we developed mental health, learning disability and autism and dementia strategic plans. These will support our services to improve clinical practice and reduce differences in outcomes for patients with these conditions.
- Deliver the pre-hospital PROMPT training to senior clinicians for safer maternity and neonatal care provision for the perinatal population of the North West.
Pre-hospital practical multi-professional training (PROMPT) is a multi-professional obstetric emergencies training programme that focusses on the out of hospital environment in providing maternity and newborn care. During 24/25 we have been working through the options available to meet the training needs of our frontline staff to be able to manage safely and effectively obstetric and neonatal emergencies. An options appraisal document is now complete and ready for review.
Patient centred care
Patient centred care means listening to and understanding what matters most to patients. To achieve this, we need to become partners in care where patients feel informed, listened to, respected and involved in the decision making around their care.
- Establish a patient safety partner policy and integrate our patient safety partners into our organisation through safety governance and improvement.
We value the contribution of Patient Safety Partners (PSPs) who are lay people who partner with us to improve safety and have a unique range of experiences to share. NWAS has recruited three PSPs to date from within the Patient and Public Panel and orientated them to the role through training (both mandatory and specialist training), monthly welfare meetings and scheduled individual meetings. The PSPs continue to develop the role through attendance at safety governance meetings including Learning from Deaths, Patient Safety Event Cases (PSEC) and Regional Clinical Learning and Improvement Group (RCLIG). They continue to support us with safety improvements, such as those made to duty of candour. It is envisaged this role will expand further with support from leaders in the organisation. We also hope to expand the number of PSPs we have in the trust during 25/26 with a focus on those who may find it difficult to access our services.
- Evaluate the benefits of the electronic patient record (EPR), access to GP records and connection of information including the barriers to uptake.
Whilst a great deal of progress has been made against this priority, there have been some unavoidable delays due to the technical readiness of the pan regional information sharing mechanism (PRISM). Work already done has identified the clinical information that does and does not provide benefit to our clinical hub to make the right decision. This will support us in understanding where we focus on external data integration in future.
- Scale up direct electronic referrals into primary care from a patient’s home.
Work with the integrated care boards has progressed steadily during 24/25 with the aim of increasing the number of direct referrals into primary care from patient’s home. Whilst this is not yet fully adopted, work is continuing into 25/26.
Quality standards and compliance
Maintaining quality standards and compliance means having the right systems and processes in place within the organisation to ensure a consistent approach to quality and quality improvement whilst adhering to external regulations responsible for monitoring quality standards within the service protecting our people, partners and patients.
- We will ensure we maintain a ‘Good’ CQC rating and conduct a developmental ‘well-led’ review and action plan to get to CQC ‘Outstanding’ within three years.
There is good evidence through board assurance that we are maintaining standards that contribute a ‘Good’ CQC rating. Plans to complete a well-led review with an accompanying action plan to achieve ‘Outstanding’ within three years, have been delayed but are now in progress with a well-led review planned for Quarter one and two in 2025.
- We will ensure we can deliver safe systems of work for staff in line with the health and safety executive standards, focusing on reducing violence and aggression towards staff and avoidable musculoskeletal injuries.
There has been a sustained improvements in compliance with reportable events being reported to the Health and Safety Executive (HSE) under the Reporting of Injuries, Diseases and Dangerous Occurrences (RIDDOR) regulations in accordance with timeframes set out in law. There has been continued innovative improvements with the DCIQ (incident reporting) system to support with timely reporting to the HSE. We have also improved our mandatory training which is designed through current data collection of incidents to make it bespoke to the incidents staff are facing.
Continuous improvement
Quality in healthcare is not static. Ensuring the care we provide remains safe, effective and person centred amidst change requires our people to have the skills, knowledge, resources and support to be able to adapt and continuously improve the care we provide.
- We will use the NHS IMPACT baseline self-assessment to work on building capability and capacity for improvement and creating the conditions for continuous improvement from the board to the frontline.
The NHS IMPACT framework was introduced by NHS England to build organisational continuous improvement. Improvement teams have been working with teams to map progress against the NHS IMPACT (Improving Patient Care Together) baseline self-assessment during 24/25. Whilst more individuals have been introduced to improvement science, to increase improvement capability at scale will require a three to five year programme. Plans on working to achieve this goal are in development.
- All teams and departments will produce a local quality improvement plan focused on safety, effectiveness, patient centeredness and patient experience improvement.
Whilst there is good evidence of improvement plans being developed and 24/25 has seen significant improvement work across NWAS at a trust-wide level, the links between local quality data and local improvements needs maturing as we move into 25/26.
- We will launch our improvement academy, aligned to strategic priorities for the ten teams who will complete their training in February 2025.
The NWAS Improvement Academy was launched in September 2024 with the first cohort comprising of six NWAS teams and two Blackpool hospital teams. A celebration event showcasing the projects supported by the Academy took place in April 2025. Feedback has been overwhelmingly positive with participants reporting that their knowledge of quality improvement methodology has demonstrably increased which is reflected in direct improvements made because of participants projects. Funding for a further cohort in 25/26 has been agreed.
- We will roll out digital innovations via the smart stations scale up, to improve the efficiency and effectiveness of operational delivery.
This has provided learnings which need to be implemented with the future process around moving innovations into projects and how innovations start and align to the trust strategy.
- We will undertake a full review of integrated performance reporting (IPR) to ensure we optimise access and insight for assurance, operational management and improvement.
The discussions on the purpose of the IPR and how it supports us to mature the organisation has been important for setting the direction for the Data Insights and Intelligence team. This has led to the development of an objective to provide support to decision makers on how to utilise data to make informed decisions.
Equality, diversity, and inclusion
To be able to create an atmosphere where all individuals feel safe, included, respected and able to flourish, it is essential to interconnect the concepts of equality, diversity and inclusion. Equality is about ensuring people are treated the same regardless of their background or characteristics. Diversity is about valuing the differences between individuals and inclusion is about creating an environment where everyone feels respected and able to contribute.
- Focus on improving learning from complaints and patient safety incident response framework (PSIRF) for patients from protected groups.
The Resolution team can now analyse the equality diversity and inclusion information captured through the complaint process. Themes are reported to Quality and Performance Committee and at the Diversity and Inclusion Group.
- Ensure all information asset owners prioritise the inclusion of protected characteristics in their system configuration, and work with the digital team to prioritise the review of data by characteristic/ deprivation.
Work has progressed in earnest to ensure the inclusion of protected characteristics are included in all system configurations. Work has been undertaken to connect data together to ensure meaningful reporting is available.
- Increase research funding to support undertaking research on reducing health inequalities.
A record level of research delivery was achieved within NWAS in 24/25 with the trust achieving its highest level of recruitment to the NIHR (National Institute of Health Research) Portfolio. This recruitment was not specifically targeted at research around health inequalities, rather delivered across a broad range of emergency and urgent care themes, however health inequalities will continue to be a focus of work across the organisation.
Our operational performance
Integrated Contact Centre (ICC)
The ongoing integration of the patient transport services (PTS), 999, and 111 contact centre services into a fully integrated contact centre (ICC) is an ambitious and crucial initiative for improving operational efficiency and patient care. The progress made in 24/25 is significant, particularly with the completion of phases one and two and the preparation for phase three of the service delivery model review.
The proposals for the phase three final structure of the integrated contact centre were approved in January 2025, and the project is now in the mobilisation stage. This final phase will be critical to completing the structural changes and embedding the integrated teams in 25/26.
Embedding the senior leadership team into the new structure is a key priority for ensuring that the integration is managed effectively. Continuing to embed joint governance procedures is crucial to maintain consistency across all three services and to ensure that integration happens in a structured, compliant, and efficient manner.
Across all areas, reductions in sickness and turnover indicate that the integration is having a positive impact on workforce stability. Increased positive feedback from staff surveys further reinforces the success of the integration progress so far. This is a key sign that the changes are not only benefiting the service at an operational level but also improving the workplace environment and culture.
Activity and demand: NHS 111
111 calls
During 24/25, NHS 111 calls answered by NWAS for the North West fell by 19.6% when compared to the previous year. A significant factor in this was due to external support given to the Trust. The support given, allowed the service to improve its workforce metrics such as reducing sickness and turnover rates, which directly contributed to better call handling and overall performance.
During 24/25, 83% of calls were answered within 60 Seconds. This represents a 33% point improvement compared to the previous year. Faster response times are crucial for patient satisfaction and ensuring that urgent cases receive immediate attention.
With support, call abandonment rate reduced by 10%, a reduction to 2.7% in abandoned calls is a great achievement, showing that the service is better equipped to handle the volume of calls, and fewer patients are left waiting or choosing to disconnect. Overall performance improvement for call pickup and workforce efficiency improved, which is crucial in the ongoing discussions regarding funding and appropriate contracts with commissioners.
Support ceased in February 2025, whilst this has represented an increase in volume for the service, we have managed to maintain strong performance, especially for call abandonment (still well within the target of under 5%).
Activity and demand: paramedic emergency service (PES)
999 call demand
In 24/25, 999 call demand has fallen by 0.7% overall compared with 23/24. However, there have been periods of variation based on external factors, for example winter pressures. Some patients have been more appropriately signposted by call handlers to alterative pathways. This in turn, reduces the number of subsequent calls received for the same patient who previously would have waited for an ambulance response.
| Fiscal year | 999 Call Demand | % difference to previous year |
| 21/22 | 1,632,595 | ↑ 26.7% |
| 22/23 | 1,531,958 | ↓ 6.2% |
| 23/24 | 1,446,700 | ↓ 5.6% |
| 24/25 | 1,436,333 | ↓ 0.7% |
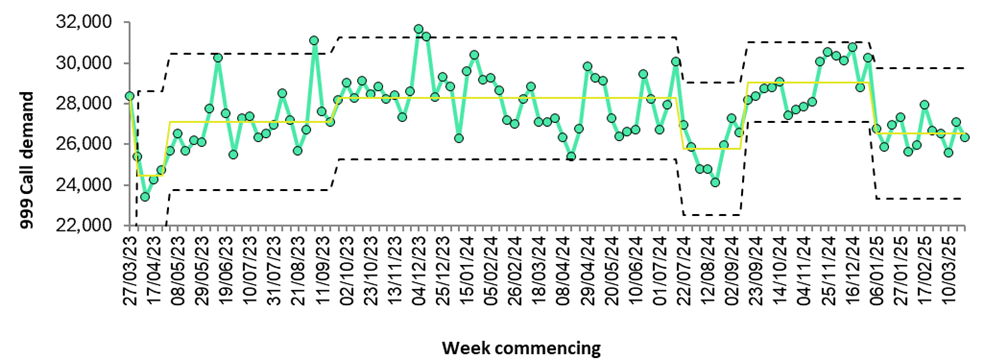
The statistical process control chart in figure 1 shows a sharp rise in demand in the baseline year (August 2024) throughout the winter where excess demand from seasonal flu for example increased demand across the whole NHS. The demand reduced in January 2025 and has been more stable in the first quarter of 2025, like the previous year.
Incidents requiring a response
In 24/25, 999 emergency incidents requiring a response has decreased by 0.3% overall compared to 23/24. The number of incidents responded to is less than the number of 999 calls received for several reasons. These reasons include multiple telephone calls being received for the same incident, estimated time of arrival enquiries and solving the patient’s needs through telephone triage and signposting to more appropriate services.
| Fiscal year | Emergency Incidents | % difference to previous year |
| 21/22 | 1,129,193 | ↓ 1.1% |
| 22/23 | 1,074,933 | ↓ 4.8% |
| 23/24 | 1,121,403 | ↑ 4.3% |
| 24/25 | 1,118,433 | ↓ 0.3% |
Within the data, there are periods within the year where call pick up has dropped below the control limit on specific dates on example July 2024 and November 2024, cause of which have been periods of high demand or a business continuity event e.g. unplanned loss of Category 3 Command and Control system meaning call handlers reverted to taking 999 calls on a paper which in turn increases call length, impacting performance. It is of note that NWAS has finished the fiscal year 24/25 with a one second 999 call pick up average (mean) with NWAS continually being ranked in the top two ambulance trusts nationally for call pick up.
Call pick up, is a vital safety metric for patients with the most life-threatening conditions (category 1) as cardiopulmonary resuscitation advice over the telephone is a critical success factor in survival. In 24/25, 999 call pick up within five seconds improved further from previous years.
| Fiscal year | % of calls answered in five seconds | % point difference to previous year |
| 21/22 | 75.9% | ↓ 19.1% |
| 22/23 | 72.8% | ↓ 3.1% |
| 23/24 | 96.8% | ↑ 24.0% |
| 24/25 | 97.8% | ↑ 1.0% |
Ambulance response programme
Ambulance service emergency performance is measured through the Ambulance Response Programme (ARP), which aims to make sure patients are reached as quickly as possible depending on their need. Under ARP there are four categories, with category 1 being the most serious, life-threatening incidents. All categories have a performance standard based on the time it takes to respond to the incident. These performance standards can be seen below:
- Category 1 is for calls about people with life-threatening injuries and illnesses. We aim to respond to these in an average time of seven minutes and at least nine out of ten times within 15 minutes.
- Category 2 is for emergency calls. We aim to respond to these in an average time of 18 minutes and at least nine out of ten times within 40 minutes.
- Category 3 is for urgent calls. In some instances, patients may be treated by ambulance staff in their own home. We aim to respond to these within 120 minutes at least nine out of ten times.
- Category 4 is for less urgent calls. In some instances, patients may be given advice over the telephone or referred to another service such as a GP or pharmacist. We aim to respond to these at least nine out of ten times within 180 minutes.
- Category 5 – Signposting advice only, no response time applies.
Response to high acuity category 1 calls has improved in 24/25 and shows a sustained improvement over time. As these are the most serious and life-threatening of calls received, ambulance services prioritise their response to these patients to save lives.
There has also been improvement in the response to category 3 and 4 patients for the second year in a row in 24/25, meaning that the response to those lower acuity calls is being provided quicker than any time since before the pandemic.
Response times to category 2 calls has increased in 24/25, despite increases in deployed ambulance resources. This increase has been driven by an increase in hospital handover times, impacting on the availability of ambulance resources to respond to patients who need a face-to-face response. Whilst the mean category 2 for 24/25 was just over one minute longer than 23/24, at 29 minutes and 49 seconds, it was within the revised recovery target set by NHS England of 30 minutes. Work is underway to reduce the category 2 response time in 25/26 with additional investment from NHS England to increase frontline resources, further support to reduce handover times, and extra clinicians in the integrated contact centre to support the triage of calls.
Whilst during 24/25 NWAS responded to slightly fewer incidents than the previous year, more incidents than ever before were managed without the need to transport a patient to hospital. Patients were provided care over the telephone, referred to another service (such as community pharmacy, community response, or their own GP), or managed at home with a face-to-face response from an ambulance service clinician.
Hospital handover
Extended time from ‘arrival to handover’ continues to be a challenge across the NWAS footprint. The average amount of time it has taken for an ambulance crew to hand over the care of a patient to the emergency department staff after the arrival at the hospital has increased from 23/24.
However, we have reduced the time taken after the patient is handed over to complete any paperwork and prepare the ambulance for the next emergency call. This ‘handover to clear’ time has been consistently below 10 minutes each month on average for the whole year.
‘Arrival to handover’, and ‘handover to clear’, when taken together give us our overall turnaround time. The increase in the average arrival to hand over time, with the small decrease in handover to clear time, means overall turnaround time has increased in the North West in the last 12 months. Some improvement has been seen in quarter four of 24/25 with significant focus on turnaround times by our integrated care board (ICB) and NHS England partners.
Work continues closely with integrated care board partners, and with individual acute hospital trusts to improve handover. Over the last 12 months NWAS has deployed ambulance liaison officers to our busiest hospitals to help coordinate the release of ambulances, has used cohorting (a process where one ambulance crew looks after a few patients to free up other crews) to allow us make crews available for further calls, and teams have taken part in collaborative work with partners to review handover processes. This has delivered some success in the later months of the financial year, and it is expected that this work will continue into 25/26 to deliver handover times closer to the target of 15 minutes, and with a nationally mandated maximum time of 45 minutes.
Arrival to handover times is higher in Cheshire and Mersey than they are in the other integrated care board areas. There has been extensive engagement across the Cheshire and Mersey ICB area throughout the year to address this, including the development of several schemes to further reduce emergency department (ED) attendance and avoid long waits, and this is now starting to show some sustained improvement.
Releasing ambulances promptly on arrival at hospital increases the availability of ambulances and improves the trusts capacity to respond to emergencies. This is why there has been significant focus from the leadership teams across NWAS, and from our ICB and acute hospital trust partners in reducing handover times.
Outcomes
All three areas of NWAS have been working with their respective ICBs around handover improvement. The three main North West ICBs all have a handover improvement working group, bringing together the acute hospitals, wider system partners, and senior leaders from NWAS to collaborate on handover improvement. These groups have been focused on improving flow through emergency departments (ED) to allow improvement in flow into the departments from waiting NWAS crews. Although the approaches have been different in the three areas, handover improvements have been delivered at some of the most challenged hospital sites in quarter four of 24/25.
Work has also been ongoing with the ICB in North Cumbria as part of some joint work between the North West and North East ambulance services. This has focused on improving escalation when delays are experienced at acute hospital sites. Plans are in place to continue this work with all the ICBs into 25/26, supported by the NHS England regional team, with a focus on improving average handover times and decreasing long waits. Improvement trajectories have been set for all the main acute hospital sites, and the local NWAS team will work with their hospital partners towards achieving these.
Urgent and emergency care growth
Additional non-recurrent funding was received in 24/25 to support the improvement of our response to category two patients. This allowed the deployment of additional ambulance hours across the footprint of the North West region. We added an additional 31 frontline staff (paramedics and emergency medical technicians) deploying 400 extra hours of ambulance time per week. Most of this additional resource was placed in Cheshire and Mersey to support demand there, but there was also extra ambulance hours added in Cumbria and Lancashire, and Greater Manchester.
The additional hours were provided to support the achievement of the interim recovery response requirement for 24/25 of a mean response time of 30 minutes to category two calls (in place of the national 18-minute mean standard), which we achieved. The funding also allowed us to provide additional supervisory support to our frontline staff. This helped us provide clinical supervision and make sure our paramedics and emergency medical technicians were supported to provide the best care possible.
Patients we help on the telephone (hear and treat)
The Integrated Contact Centre (ICC) clinical delivery team has been working hard to improve the process of treating patients over the phone, helping reduce unnecessary ambulance dispatches. During 24/25, 15% of emergency incidents were managed through triage and treated over the telephone.
Positive impacts of ‘hear and treat’ include:
- Reducing ambulance demand. By addressing more cases via telephone, fewer ambulances are required which can help prioritise emergency resources for patients in more urgent need.
- Improving efficiency. Streamlining the triage process helps make better use of time and resources, improving the overall efficiency of the healthcare system.
- Cost savings. Treating patients over the telephone reduces operational costs associated with ambulance dispatch and emergency department visits.
- Patient satisfaction: For some patients, being treated at home through telephone triage can be more convenient and less disruptive, enhancing overall satisfaction with the service.
Patients not conveyed to hospital (see and treat)
As there is improvement in ‘hear and treat’ rates, ambulances are only sent to the patients that cannot be helped on the telephone, and these are often more complex or unwell patients. Some of the patients attended with a face-to-face response may still be assessed by a clinician and be identified as being suitable for management by a primary care service or urgent care service rather than needing transportation to an emergency department. This is referred to as ‘see and treat.’
Working closely with partners in heath, social care, and the third (voluntary and not-for-profit) sector, pathways have been developed that provide the care required without the need for the patient to be taken to hospital. This includes access to virtual wards, response within two hours by urgent care clinicians based in the community, or specialist community pathways for frail patients, or those with specific conditions such as respiratory illness. These are just some examples of pathways that NWAS clinicians can access to support managing patients in places other than at hospital.
In 24/25 there was a small reduction in ‘see and treat’ rates, which is likely to be due to more patients being managed through assessment over the telephone and not needing a face-to-face response. In 25/26 there is planning for further work with system partners to find additional appropriate ways of managing patients in the community who do not need transporting to an emergency department. This will include coordination of the care offered at place level by system partners, making it easier for an NWAS clinician to access the right solution for a patient. This will help to lessen demand on busy emergency departments and support providing the appropriate care for patients closer to home, or in the patient’s home.
Leadership review
Over the last 12 months a new frontline operational and clinical leadership structure has been implemented across the service delivery directorate. As well as delivering a focus on team management, supervision, and support for frontline staff, it has enhanced our response to patients. There are now a minimum of six advanced paramedic practitioners with skills in managing critically unwell and complex patients on duty across the region 24 hours a day. They respond to patients that need additional advanced skills and knowledge such as complex maternity, acutely unwell paediatric patients, serious trauma, and cardiac arrests. There are also six duty officers, our first line operational leadership response to incidents, available across the region 24 hours a day. They provide support at multi-patient incidents, our operational commander response to significant and major incidents, and welfare and wellbeing support to crews who attend difficult incidents. The changes have also seen the introduction of sector clinical leads who work closely with the wider local management teams to improve and sustain the quality of care delivered by frontline clinicians.
The review has also increased our ability to respond to the most critically unwell patients in a timely manner, and this has already led to a small improvement in mean category one response times, with more work being undertaken to further improve these in 25/26.
Activity and demand: Patient transport service (PTS)
The patient transport service (PTS) contracts for Merseyside, Greater Manchester, Lancashire, and Cumbria were due to expire in 2024. These were initially extended to 31 March 2025. During 24/25 NWAS re-submitted bids for the new contracts for the period 25/30 across three lots; Cheshire and Merseyside, Greater Manchester, and Cumbria and Lancashire and the contract was subsequently extended until 31 March 2026.
The outcome of this second procurement exercise was expected on 31 January 2025. Notification was received that commissioners had decided not to award a contract, and the current contract was to continue until 31 March 2026. NWAS is awaiting further information regarding the next steps for the procurement and contracting arrangements for 26/27.
In September 2023, the PTS senior leadership team agreed a financial improvement plan to be delivered by 31st March 2025. The overarching objective was to optimise patient journeys whilst delivering financial efficiencies. Key deliverables of the plan included:
- Reducing the use of private ambulances across the service: through quarters one to three, the use of private ambulances reduced by over 50% per day. This resulted in a greater proportion of contracted activity delivered through NWAS resources throughout 24/25, also improving effective use of resources.
- Recruitment of an additional 130 volunteer car drivers: whilst the ambitious target was not achieved, an additional 60 volunteers were recruited with 70 more in the recruitment process. Positively, the total number of volunteer car drivers increased from 128 in 23/24 to 162 in 24/25. The contributions of these volunteers is invaluable and we are extremely grateful for the support the give to us and their communities.
PTS performance activity
| Contract | 24/25 Baseline | 24/25 Activity | Activity Variance | Activity Variance % |
| Cumbria | 168,290 | 135,886 | -32,404 | -19% |
| Greater Manchester | 526,588 | 568,461 | 41,873 | 8% |
| Lancashire | 589,181 | 439,661 | -149,520 | -25% |
| Merseyside | 300,123 | 314,438 | 14,315 | 5% |
| NWAS | 1,584,182 | 1,458,446 | -125,736 | -8% |
PTS activity in 24/25 has continued to grow and is now sitting around 8% below the baseline compared to 10% below the baseline in 23/24. Although Merseyside and Greater Manchester saw an increase in activity of 5% and 8% respectively above expected levels, Lancashire experienced a reduction of 25% and Cumbria a reduction of 19% against expected activity levels. The increase in activity has been delivered in the context of diverse and evolving healthcare systems, with reconfiguration of hospital services, an increasing number of locations over geographically spread greater distances, with increasingly complex patients, and reducing dependence on third-party providers.
It is essential to maintain an efficient and effective balance that ensures PTS meets the needs of patients, the local hospital trusts and integrated care systems whilst delivering a high quality, responsive and financially viable service.
Utilisation
As planned in the previous year the focus for PTS in 23/24 was to return to pre-covid utilisation of 1.8 patients transported per hour in an average eight-hour shift. During Covid, this utilisation dropped to 1.2 due to single occupancy of our vehicles although Covid positive patients could travel together resulting in utilisation occasionally being above 1.0.
Although the objective was to return to pre-covid utilisation rates of 1.8, analysis has shown that since 18/19 the healthcare system has changed in relation to outpatient services. Patients are now travelling to more locations further afield, meaning that the dynamic use of resource can be challenging. Throughout 24/25 utilisation has improved and there has been an upward trend for all counties with Merseyside showing the greatest improvement at 1.51 at the end of March 2025.
PTS improvement programme
The PTS service line continues to make progress in terms of its priorities and maintaining a high quality of service to our patients. However, to make sustainable improvements against these priorities a refreshed PTS improvement programme of work was commissioned by the Trust Management Committee. This improvement programme, initiated in November 2024, builds on the work delivered in the PTS financial improvement plan (23/25).
The improvement programme is designed to improve outcomes and experience for patients and staff whilst ensuring delivery of the contractual obligations and financial efficiencies. The work streams will deliver a modern-day logistics operation, set against the backdrop of a combination of increasing activity, increasing places of care and more stringent performance standards.
The improvement programme is an 18-month programme of work that facilitates a collaborative approach from across NWAS with all subject matter experts, to resolve some of the challenges faced by PTS, focusing on:
- Digital solutions and innovations
- Workforce and leadership development
- Improving operational productivity and efficiency
- Improving culture
- Financial efficiency as a bi-product of the above.
Patient safety
Maintaining the safety of our vulnerable patients remained a priority throughout 24/25. PTS continues to trial the Furno Power Trax, tracked chair which, if successful, will enable safer movement of patients up and down stairs whilst maintaining the safety of our staff in terms of manual handling. New standard operating procedures were also introduced to respond to safety legislation in the transporting of patients in wheelchairs.
PTS also trialled an electric vehicle and the feedback from patients was very positive. They said that it was a much smoother and more comfortable ride. This is a positive trial for future development of the PTS fleet.
In 24/25 we committed to recruit a PTS clinical quality lead and the new post holder will start shortly. The role will focus on clinical, quality, and governance initiatives within the service, shaping and enhancing patient transport delivery, ensuring compliance with regulatory standards and driving continuous improvement across clinical operations.
Digital developments
In 24/25 the ‘text NO to cancel’ service was introduced. This service made use of the 3 automated text messages sent to patients:
- Booking confirmation
- Three days’ notice
- Vehicle on route
Patients can reply to the text message with a simple ‘NO’. This will result in the patient’s booking being cancelled or aborted if the vehicle had committed to collect them. This should result in an improved patient experience through reduction in calls to cancel transport and productivity improvements due to a reduction in aborted journeys. Analysis of the impact of this new service is ongoing.
Development across all three service lines, PES, 111 and PTS saw the introduction of a notification to the PTS service if the patient, identified by NHS Number, had made a call to 999 or 111 within the previous 24hrs. The purpose is to allow PTS dispatch to enquire if the planned PTS transport was still required. This is a new innovation and the impact of it is yet to be assessed but is expected to show a reduction in the number of cancelled and aborted journeys if patients have been admitted to hospital.
Recruitment to senior management positions in the PTS leadership team will conclude shortly as will recruitment to PTS team leader roles. These will fully establish frontline supervision and provide much needed support to our staff both operationally and in terms of visibility and engagement.
Performance and quality standards: Patient transport services (PTS)
There are four areas of quality performance indicators within the patient transport service known as quality standards
- Call answering
- Travel time on a vehicle
- On time arrival
- Collection after treatment
These performance indicators are measured based on whether the journey was planned or unplanned, or if the journey was for someone receiving enhanced priority service (EPS) including renal dialysis, or cancer treatment).
| PTS Contractual Quality Indicators 24/25 | 24/25 performance |
| 75% of calls answered within 20 seconds | 27.8% |
| Average length of time taken to answer inbound calls (Average is 60 seconds) | 04:57 (seconds) |
| Planned Care: 85% passenger time on vehicles is less than 60 minutes | 86.3% |
| Planned Care: 90% of patients arriving within 60 minutes of scheduled appointment time | 76.7% |
| Planned Care: 80% of patients collected within 60 minutes of scheduled collection time or patient readiness notification | 58.3% |
| Planned Care: 90% of patients collected within 90 minutes of scheduled collection time or patient readiness notification | 79.0% |
| Unplanned Care: 80% passenger time on vehicles is less than 60 minutes | 88.6% |
| Unplanned Care: 80% of journeys where the patient is picked up no later than 60 minutes after booked collection time | 55.4% |
| Unplanned Care: 90% of journeys where the patient is picked up no later than 90 minutes after booked collection time | 68.9% |
| Enhanced Priority Service: 85% passenger time on vehicles is less than 60 minutes | 91% |
| Enhanced Priority Service: 90% of patients arriving 45 minutes prior to scheduled appointment time | 76.0% |
| Enhanced Priority Service: 85% of patients collected within 60 minutes of scheduled collection time or patient readiness notification | 78.7% |
| Enhanced Priority Service: 90% of patients collected within 90 minutes of scheduled collection time or patient readiness notification | 92.0% |
Our quality assurance
Ambulance quality indicators (AQIs)
A key measure of the effectiveness of our services is the monthly National AQI submission to NHS England, produced by the Clinical Audit team. This is then utilised by clinical leadership teams to work with system partners to learn and share outcomes and ultimately informing local improvement workstreams.
We provide quarterly AQI reports to the Clinical and Quality Group and Quality and Performance committee. We provide further localised reporting for STEMI (ST segment elevation myocardial infarction, a heart attack confirmed from the heart trace) and reporting of older adult falls, to our clinical leads, to contribute to learning and improvement.
| National Ambulance Quality Indicators | April-November performance 23/24 | April-November performance 24/25 | April-November national average 24/25 |
| Cardiac arrest (all-ROSC at hospital) | 32.7% (829/2,532) | 29.7% (771/2,597) | 27.9% (5,830/20,913) |
| Cardiac arrest (Utstein-ROSC at hospital) | 50.6% (221/437) | 51.9% (246/474) | 51.0% (1,639/3,212) |
| Post ROSC care bundle | 74.8% (294/393) | 87.8% (310/353) | 83.7% (2,366/2,827) |
| Cardiac arrest (all-survival to 30 days) | 10.8% (270/2,497) | 10.5% (270/2,577) | 10.2% (2,112/20,730) |
| Cardiac arrest (Utstein-survival to 30 days) | 28.9% (1233/425) | 28.3% (131/463) | 30.3% (955/3,149) |
| STEMI care bundle | 75.1% (446/594) | 90.7% (568/626) | 78.2% (4,047/5,174) |
| STEMI PPCI patients (call to angiography) | 02:28:00 (627) | 02:35:00 (1,082) | 02:30:00 (8,658) |
| Confirmed stroke patients (call to door) | 01:23:00 (4,598) | 01:19:00 (3,532) * | 01:33:00 (26,686) * |
| Older adult falls care bundle | N/A | 19% (114/300) | 43.8% (2671/6097) |
NB. ROSC means Return of Spontaneous Circulation and PPCI refers to an urgent hospital procedure to reduce heart damage.
*Stroke (SSNAP) data currently only available nationally up to September 2024 due to implementation of new webtool
Data collection for these indicators occurs three months in arrears. Following a successful pilot during 23/24, the older adult falls AQI has been introduced to the national AQIs. Whilst NWAS sits below the national average for this AQI, there has been a significant amount of work that has gone into increasing compliance such as, face-to-face training through the trust’s mandatory training cycle and the introduction of a falls tile within the Electronic Patient Record (EPR) which provides structure and prompts for clinicians. Whilst this isn’t yet reflected in the performance data that has been published to date, we know that it is positively impacting performance, and we should continue to see improvements across quarter four data and into 25/26.
Additionally, both ST segment myocardial infarction (STEMI) and post return of spontaneous respiration (ROSC) care bundles have increased from last year’s data and are above national average. This is because of changes to the trusts EPR system for STEMI care and focused stretch targets for post ROSC care that took place towards the end of 23/24 with that data showing sustain improvements through 24/25.
We have submitted 100% eligible cases for the national AQIs and to eligible national clinical audit projects including the myocardial (heart) ischaemia national audit project (MINAP) during April-November 2024. In relation to the sentinel stroke national audit project (SSNAP); which is another national clinical audit project, a newly implemented webtool in September 2024 has prevented ambulance trusts from submitting cases since then. This is something that is being worked on to resolve, however, prior to September 2024, 100% of eligible cases were submitted.
Learning from deaths
Our approach to learning from deaths goes far beyond a process of simply counting, classifying and reporting deaths. This process aids in protecting future patients from avoidable harm, reduce unwarranted variation and provide truly patient-centred care. This involves a structured methodology to review each case, encompassing senior clinician review, peer to peer moderation and thematic analysis of any lessons learnt. This allows the identification of both areas of improvement and areas of excellent practice which is shared across the trust through established learning forums and internal communication routes. This is further supported by our patient partners, ensuring that our patient voice is involved and heard during this delicate and often difficult process.
In the past year we have once again met all reporting requirements. We produce quarterly learning from deaths reports, reviewed by Clinical and Quality Group, Quality and Performance committee and Board.
The table below details the number of deaths reviewed and the number of deaths where problems in care have contributed.
| Fiscal quarter | Total number of deaths in scope | Total number of deaths reviewed | % of deaths reviewed | Total number of deaths where problems in care have contributed |
| Q1 | 66 | 29 | 43.9% | 5 |
| Q2 | 62 | 41 | 66.1% | 15 |
| Q3 | 98 | 56 | 57.1% | 9 |
| Q4 | Not available at the time of publication | |||
| Year-to-date | 226 | 126 | 55.8% | 29 |
The key areas of good practice continue to be:
- Recognition of patients at the end of life and working with patients, families and multi-disciplinary teams to ensure that there are appropriate advanced care plans in place to ensure high quality care to patients.
- Making patient centred decisions around patients remaining at home with appropriate safety netting and advice regarding what to do if condition worsens.
- Within contact centres our call handling teams can seek advice when concerned around patients they’re assessing or when dealing with complex calls.
Areas of learning and improvement:
- Poor Electronic Patient Record (EPR) quality has been a consistent theme which has meant that it is challenging to know what assessments and advice were given and whether they were appropriate.
- Lack of structured clinical assessment models.
- Detail within mental capacity assessments.
- Probing within ICC call handling.
Themes and trends that are identified through the structured judgement reviews (SJR) are fed into area learning forums and additionally this year they are all feeding into the Integrated Contact Centre (ICC), Incident Learning and Improvement Forum as well as the Regional Clinical Learning and Improvement Group (RCLIG).
For some of the themes mentioned above, work is already underway to address these issues, such as probing workshops within the ICCs, or mental capacity forming part of the upcoming Patient Safety Incident Response Framework (PSIRF) priorities. Where there is no work currently underway, workstreams are forming through RCLIG to drive improvements for example, reviews of EPR quality in a wider context outside of learning from deaths to explore this further and consider what improvements can be made.
The completion of the service model delivery review (SMDR) has also seen some changes to the membership of the structured judgement review (SJR) moderation panels. The SJR panel is comprised of a group of our sector clinical leads, with support from our Clinical Audit team and patient partners, chaired by a consultant paramedic. It is an open meeting, meaning that any member of clinical staff can attend and participate in the moderation, and this allows for both patient and frontline staff opinions and views to be heard and considered when making decisions on patient outcomes.
We have been working with the sector clinical leads to provide them with an introduction to this process to enable them to continue to support the work of learning from deaths. We have also been working with the ICC teams to ensure that the call handling support that has been provided to this work continues, following the completion of their organisational changes which are ongoing.
Prevention of future deaths
A regulation 28 report is a report issued by a Coroner if they identify concerns that, if addressed could prevent future deaths. We aim to receive a very low number of Regulation 28 Prevention of Future Death reports as we proactively and continuously seek opportunities for improvement.
Upon receipt of a Regulation 28 Prevention of Future Death report, we endeavour to ensure that all learning actions which may arise from a coroner’s investigation are identified promptly and proactively completed in a timely manner. During 24/25, we received two Regulation 28 Prevention of Future Death reports. The report and our responses are published on the chief coroner’s website. In summary:
- 10 April 2024: Issued by Manchester North assistant coroner in relation to a patient who had taken an overdose, and who subsequently could not be contacted by a clinician for a further clinical assessment by telephone. The coroner was concerned that there was no escalation process for unanswered calls especially when the patient could be unconscious/deceased.
- 2 October 2024: Issued by Manchester South assistant coroner issued in relation to a lack of probing by the mental health practitioner during a telephone triage in the days prior to the patient’s death, which resulted in a missed opportunity for a face-to-face assessment.
We have responded to the Regulation 28 Prevention of Future Death reports. Our responses are published on the Courts and Tribunals Judiciary website.
We strive to provide high standards of care for our patients and service users. Compliments are a source of pride that are very important to our people. Compliments provide us with an opportunity to feedback to colleagues in recognition they deserve for truly making a difference to patients’ lives. A total of 1,150 compliments were received during 24/25. Some compliments received are attributed to multiple service lines, hence the variation in numbers.
Compliments
| Service Line | Cheshire and Merseyside | Cumbria and Lancashire | Greater Manchester | Total |
| Paramedic emergency service (PES) | 492 | 300 | 330 | 1122 |
| NHS 111 | 30 | 30 | 33 | 93 |
| Emergency operations centres (EOC) | 17 | 6 | 13 | 36 |
| Patient transport service (PTS) Operations | 5 | 2 | 18 | 25 |
| Community first responders | 0 | 7 | 0 | 7 |
| North West Air Ambulance | 0 | 0 | 2 | 2 |
| Service delivery | 1 | 0 | 0 | 1 |
| Corporate function | 0 | 1 | 0 | 1 |
| NWAS | 1 | 0 | 0 | 1 |
| Themes | Cheshire and Merseyside | Cumbria and Lancashire | Greater Manchester | Total |
| Clinical treatment – face-to-face | 480 | 286 | 213 | 979 |
| PES response | 1 | 20 | 112 | 133 |
| Attitude and behaviour | 1 | 0 | 77 | 78 |
| Clinical treatment – virtual | 9 | 2 | 18 | 29 |
| PTS journeys | 3 | 2 | 18 | 23 |
| Communication – virtual | 7 | 5 | 8 | 20 |
| Communication – face-to-face | 13 | 1 | 3 | 17 |
| Dispatch | 2 | 0 | 1 | 3 |
| Care and treatment | 0 | 0 | 2 | 2 |
| Competence | 0 | 0 | 2 | 2 |
| Other | 0 | 0 | 2 | 2 |
| Call handling and planning | 0 | 0 | 1 | 1 |
| Total | 516 | 316 | 457 | 1289 |
Patient engagement and experience
Each year the trust’s Patient Engagement team deliver an extensive patient engagement programme in line with our Patient Public and Community Engagement Implementation Plan. The plan sets out the ways we propose to engage with and obtain feedback from our patients across all service areas, including our paramedic emergency service (PES), patient transport service (PTS), the NHS 111 service and our urgent care desk. The plan also supports the trust Quality Strategy aims of ‘person-centred partnerships’ with our patients, public and communities.
A minimum 1% of PTS, PES See and Treat patients, are offered the opportunity to provide Friends and Family Test (FFT) feedback monthly via short message service (SMS) text channel, and each week 300 NHS 111 patients receive the nationally mandated NHS 111 patient experience postal survey. We now offer predominantly digital opportunities to provide feedback using SMS text invites to deliver digital links to our online surveys. We also continue to review our quick response (QR) code feedback posters and returnable postcards on both 999 and PTS ambulances for patients to be able to provide real time feedback.
We have used a combination of virtual and face-to-face engagement methods to engage with specialist community patient groups depending on their preference. We have been able to listen to the issues and experiences of our patients from mixed diverse and ethnic communities at our five Ambulance Awareness events, university Freshers’ Fayres and other large footfall events across our footprint.
Patient experience survey and the Friends and Family Test 24/25
We provide tailored surveys across our 999, urgent care, PTS, and NHS 111 services, inviting patients and carers to share their experiences. These are reviewed annually by service teams and our Patient and Public Panel (PPP) to ensure they remain relevant.
The FFT asks whether patients would recommend our services and allows them to explain their views, offering valuable insights that guide service improvements.
In 24/25, we received over 25,588 responses, with a return rate of 7.54% – a 1.33% decrease from the previous year. The NHS 111 postal survey saw the highest return rate at 10.29%, reflecting strong ongoing engagement across feedback channels.
| Patient Engagement Survey – Survey Channels (24/25) | Completed Returns | % of Total | |
| Patient Transport Service Patient Experience Survey | Via SMS delivery – on-line completion | 1,392 | 5.44% |
| Patient Transport Service FFT | SMS text completion | 13,545 | 52.93% |
| Patient Transport Service FFT | Post cards | 541 | 2.11% |
| Paramedic Emergency Service Patient Experience Survey | Via SMS delivery – on-line completion | 912 | 3.56% |
| Paramedic Emergency Service FFT (See and Treat). | SMS text completion | 6,589 | 25.75% |
| Paramedic Emergency Service FFT (See and Treat). | Post cards | 47 | 0.18% |
| Paramedic Emergency Service FFT (Comment Card) (Conveyed patients). | Post cards | 287 | 1.12% |
| Urgent Care Service Patient Experience Survey. | Via SMS delivery – on-line completion | 482 | 1.88% |
| National NHS 111 Service Patient Experience Survey | Postal | 1,553 | 6.07% |
| Localised NWAS NHS 111 Service \Patient Experience Survey | Via SMS delivery – on-line completion | 240 | 0.94% |
| Total | 25,588 | ||
Feedback received during 24/25 shows high regard for ambulance services and particularly the care and treatment provided by staff. A high 93.4% of PTS and 90.6% of PES patients respectively stating that they were ‘cared for appropriately with dignity, respect, kindness and compassion’.
NB Fields showing ‘not applicable’ indicate that the question was not included in that survey.
| Patient Engagement Surveys | |||||
| SMS Text Delivery/Postal/On-line | |||||
| Cared for appropriately with dignity, compassion and respect (Strongly Agree/Agree) | |||||
| Q1 | Q2 | Q3 | Q4 | YTD | |
| PTS | 90.50% | 94.20% | 95.40% | 94.70% | 93.40% |
| PES | 92.60% | 89.70% | 89.60% | 90.30% | 90.60% |
| UCS | 92.60% | 91.60% | 95.20% | 94.80% | 94.00% |
| 111 | 94.50% | 97.10% | 92.50% | 95.70% | 94.10% |
| Patient Engagement Surveys | |||||
| SMS Text Delivery/Postal/On-line | |||||
| Overall satisfaction Received (Very Satisfied/Fairly Satisfied – Yes) | |||||
| Q1 | Q2 | Q3 | Q4 | YTD | |
| PTS | n/a | n/a | n/a | n/a | n/a |
| PES | n/a | n/a | n/a | n/a | n/a |
| UCS | n/a | n/a | n/a | n/a | n/a |
| 111 | 87.40% | 87.00% | 85.10% | 89.90% | 86.90% |
| Patient Engagement Surveys | |||||
| SMS Text Delivery/Postal/On-line | |||||
| Overall Experience of Service / Recommend Ambulance Service to Friends and Family (Very Good/Good – Extremely likely/Likely) | |||||
| Q1 | Q2 | Q3 | Q4 | YTD | |
| PTS | 89.10% | 91.00% | 92.10% | 91.50% | 90.70% |
| PES | 91.30% | 90.10% | 88.20% | 91.10% | 90.20% |
| UCS | 84.30% | 74.80% | 81.40% | 81.80% | 82.20% |
| 111 | 89.70% | 90.00% | 88.00% | 89.20% | 89.10% |
Examples of additional narrative in feedback include:
- “Excellent, amazing service. Extremely professional. My son is autistic, and the two paramedics went the extra mile to make sure reasonable adjustments were made to aid his recovery, kind understanding and valued my input so to get full picture of events and history. Couldn’t have asked for more in an already stretched area of the NHS. Excellent.” (PES)
- “Excellent staff very caring and kind. Just what you need after outpatients’ treatment. I truly appreciate this vital service. Thank you all. Ps. (sic) Also the lady on the phone taking the booking was kind and caring and made it so easy for me. That too was greatly appreciated.” (PTS)
- “Both paramedics were empathetic, conscientious, thorough and my partners symptoms were taken seriously in spite of them being less serious than he initially thought. We did not wait an excessive amount of time. Overall, a very reassuring/supportive experience. Credit to both paramedics and the practitioner who took the 111 calls.” (PES)
90.2% of PES patients, 86.9% of NHS 111 patients and 90.7% of PTS patients also found their overall experience of the respective services either good or very good.
- “My Mum travels to and from dialysis by ambulance 3 times a week. She is 86 and quite frail and can get a bit confused. All of the ambulance crew have taken the time to get to know her well and they are all so kind, caring and professional in their dealings with her. They have a chat and a joke with her, and she loves them all.” (PTS)
- “Amazing service from NWAS. Ellie and the team were super with my Mum who had fallen and were really kind and compassionate. They were very thorough and quickly examined my Mum, giving excellent treatment and a real human touch. They were calm, quick acting and efficient. Really went the extra mile. Thank you all so much again, really grateful for your amazing service at a very stressful time. It is really appreciated.” (PES)
- “111 knew my husband needed help. They took control of his problem. They got an ambulance to take my husband to Urgent Care Centre, he was treated straight away, on monitors, admitted to hospital. I can’t thank 111 enough, as I was panicking. They knew the situation and responded. Ambulance service, 111, all amazing. If it wasn’t for 111, my husband would not be alive today. They took complete control and responded by saving my husband’s life. We are eternally grateful.” (NHS 111)
Friends and Family Test (FFT)
PTS and PES ‘see and treat’ patients, receive the opportunity to provide FFT feedback monthly through a SMS message. Monthly FFT data is shared via the Integrated Performance Report (IPR) at Board, Quality Committee and nationally with NHS England. A thematic analysis of the FFT qualitative feedback continues to show a high regard for the professionalism, care and compassion shown by our staff. Areas of learning include delays, waiting times, and where there could be expectations for some of our more vulnerable PTS patients when using third party or bariatric services and wheelchair support.
The table below provides a breakdown of the FFT feedback data and channels used to gather patient experience. As can be seen, a high number of patients provide qualifying narrative to support their response.
| 24/25 Summary of FFT Responses and Channels | |
| FFT Responses received in 24/25 | 22,394 |
| Increase compared to 23/24 | 26.14% |
| Additional comments entered on FFT responses | 17,982 |
| SMS text survey responses | 89.14% |
| Postal postcard surveys | 2.85% |
| On-line responses | 8.01% |
Demographic analysis of patient, experience surveys and SMS text FFT
The table below shows the percentage breakdown of survey respondents by demographics for our PTS, PES, urgent care service (UCS) and NHS 111 surveys, and where we received FFT feedback via SMS on our PES and PTS service lines. Some key headlines include:
- 95.3% of PTS respondents are over 45 years of age.
- 58.9% of NHS 111 respondents are female.
- 82.8% of PTS respondents declared a disability.
- An average of 6.22% of all respondents were from ethnic minority communities.
- On average, 1.73% of all respondents preferred not to declare their ethnicity.
A continued focus for 25/26 will be to increase the amount of feedback we receive from mixed ethnic communities and to improve the capturing and reporting of demographic information and protected characteristics.
| PTS | PES | UCS | Local 111 | National 111 | PTS FFT | PES FFT | ||
| Mode of correspondence | (URL) | (URL) | (URL) | (URL) | (Postal) | (SMS Text) | (SMS Text) | |
| Patient Age | Under 16 yrs | 0.6% | 6.8% | 5.2% | 18.2% | 3.7% | 0.9% | 1.2% |
| Over 16+ yrs | 99.4% | 93.2% | 94.8% | 81.9% | 93.8% | 99.1% | 96.4% | |
| Over 25+ yrs | 99.1% | 90.7% | 90.0% | 76.0% | 91.2% | 98.5% | 93.6% | |
| Over 35+ yrs | 98.5% | 86.2% | 83.8% | 63.0% | 85.3% | 97.4% | 89.0% | |
| Over 45+ yrs | 95.3% | 79.7% | 76.3% | 51.0% | 76.8% | 94.4% | 78.8% | |
| Over 55+ yrs | 86.6% | 69.5% | 66.1% | 34.8% | 69.1% | 86.5% | 65.1% | |
| Over 65+ yrs | 65.6% | 53.2% | 50.1% | 16.2% | 55.2% | 67.7% | 42.6% | |
| Over 75+ yrs | 36.3% | 32.8% | 32.2% | 5.1% | 32.6% | 41.3% | 21.9% | |
| Over 85+ yrs | 8.5% | 9.2% | 10.8% | 0.8% | No data | 12.2% | 6.7% | |
| Patient Gender | Female | 53.2% | 53.1% | 58.9% | 57.7% | 60.3% | 55.0% | 60.3% |
| Male | 46.6% | 46.4% | 40.7% | 41.9% | 37.5% | 45.0% | 36.7% | |
| Prefer not to say | 0.2% | 0.6% | 0.4% | 0.4% | 2.2% | 0.0% | 3.0% | |
| Patient Impairment | Limiting illness | n/a | n/a | n/a | n/a | 47.6% | n/a | n/a |
| None | 17.2% | 41.2% | 46.3% | 68.2% | 47.0% | 6.3% | 37.9% | |
| More than one | n/a | n/a | n/a | n/a | n/a | 26.9% | 18.2% | |
| Mobility | 68.3% | 37.2% | 31.3% | 15.5% | n/a | 52.3% | 20.4% | |
| Hearing | 14.9% | 14.9% | 13.6% | 4.6% | n/a | 0.8% | 2.1% | |
| Visual | 8.9% | 5.9% | 4.5% | 0.4% | n/a | 3.2% | 0.7% | |
| Mental Health | 10.7% | 15.2% | 17.2% | 10.5% | n/a | 2.0% | 7.7% | |
| Dementia | n/a | n/a | n/a | 0.0% | n/a | 0.8% | 2.7% | |
| Learning | 1.7% | 3.0% | 4.7% | 3.8% | n/a | 0.8% | 1.3% | |
| Don’t know | n/a | n/a | n/a | n/a | 2.0% | 0.8% | 1.3% | |
| Prefer not to say | n/a | n/a | n/a | n/a | n/a | 6.9% | 9.2% | |
| Patient Ethnicity | (Black & Minority Ethnic Communities) | 3.9% | 5.0% | 7.3% | 8.3% | 6.1% | 5.4% | 7.6% |
| Prefer not to say | 1.7% | 1.2% | 0.8% | 0.8% | 0.0% | 2.7% | 3.2% | |
Reporting
Friends and Family Test patient feedback is reported monthly to the Board through the Integrated Performance Report and quarterly via the Communications and Engagement dashboard. Key engagement themes and initiatives are also shared with the Quality and Performance Committee, while Equality Diversity and Inclusion (EDI) updates go to the EDI Sub Committee.
In 24/25, we continued quarterly service improvement dashboards and began developing a new, combined patient feedback dashboard – an important initiative that will continue into 25/26.
Feedback themes
Feedback over the year has consistently demonstrated a generally high regard for the ambulance service and in particular the high percentage of patients feeling they were treated with dignity, compassion and respect (92.8% of survey respondents).
Some of the themes and feedback highlighted during the year have included:
- Awareness of the NHS 111, online services for those from ethnic minority groups.
- Awareness of the availability of interpretation and translations services for Deaf, black and ethnic minority communities (BAME).
- An understanding of what information may be requested when 999 is called for patients whose first language is not English.
- Profiling job roles, routes to employment and volunteering within the ambulance service at our community events.
- Increased understanding of how to improve with patients with a learning disability or autism, including the opportunity to learn basic British Sign Language (BSL).
- Staff awareness of cultural and religious differences when entering homes and the ability to provide dignity in death.
Patient and public panel – giving our patients ‘an increased voice’
Our volunteer Patient and Public Panel (PPP), established in 2019, is made up of representatives from local communities, interest groups, the voluntary sector and partner organisations. The PPP offers meaningful opportunities for members to influence decisions and identify areas for improvements in our urgent and emergency care, patient transport, NHS 111 and back-office services in a way that suits their lifestyle and the time and commitment they can give. Panel members bring expert lived experience and knowledge of our services and offer valuable insights into numerous projects, initiatives, policies, systems and campaigns.
The PPP has a flexible infrastructure to enable patients and the public to become involved at one or more levels that best suit them. All levels are equally important and consist of:
- ‘Consult’ is virtual, making the most of digital channels to interact with members
- ‘Co-produce’ panel members work together on short-term projects
- ‘Influence’ members take an ongoing, active role in high-level meetings
A breakdown of PPP members’ involvement by level can be found in the figure below.
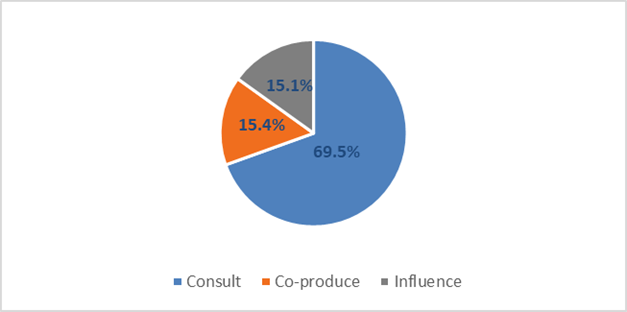
As our PPP has continued to grow over the last 12 months, we have actively engaged with our members via both face-to-face and virtual platforms with the intention of ensuring our members feel supported in the role. Our 344 PPP members are fully inducted into the organisation, with many already involved in work with the trust.
The table below shows the distribution of PPP members across the localities.
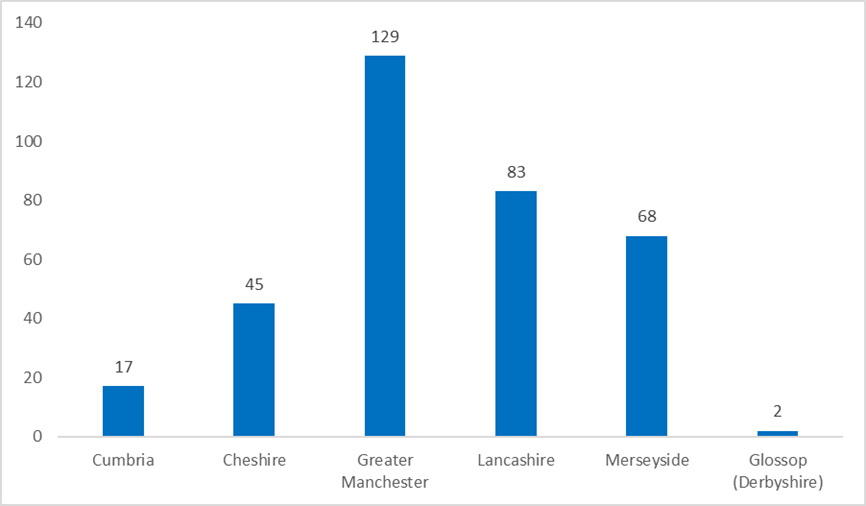
During 24/25 we increased the diversity of the panel’s membership, rising from 24% to 26% for cultural representation, 32% for youth representation and 25% for representation of patients with disabilities. The panel’s feedback and lived experience are invaluable to the trust to better understand our patients’ experience, produce stories, analysis and themed findings which in turn inform service development.
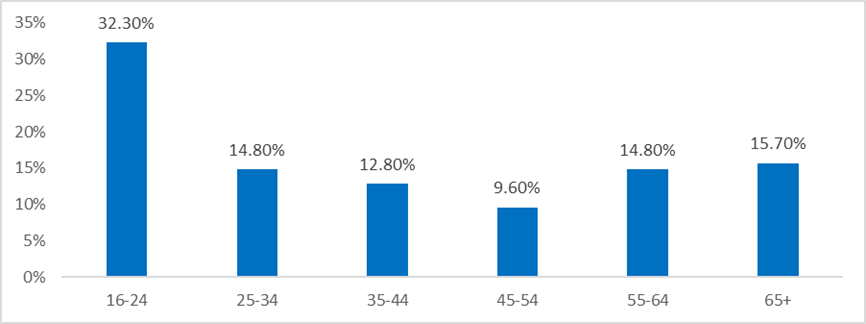
In 24/25, PPP members have been invited to join a variety of forums with 23 requests for panel involvement from staff across the trust as well as external partners such as Lancashire and South Cumbria Integrated Care Board. Areas the PPP have been involved in include regular attendance at high-level meetings such as area learning forums, attendance at trust board and learning from deaths meetings/discussions. In addition, our PPP have played a significant role in forming strategy, developing resources and supporting projects for example:
- A discussion was held with PPP members as to what they think should be included in the trust Mental Health and Dementia Strategic Plan for 24/27. The trust Mental Health leads team will be producing a separate plan for dementia and will be coming back to the PPP to help produce this plan along with others in the future.
- PPP members reviewed our pictorial e-book to help ensure each question and procedure within the book is clearly explained to support neurodiverse and learning disability patients. Feedback shared from PPP members resulted in some of the terminology changing to make it easier read and additional questions included to help neurodiverse and learning disability patients when being treated.
Panel members receive regular information via a weekly roundup newsletter, with 51 editions shared during 24/25. Some of the featured articles included Black History Month, World Menopause Day, PPP session looking at 999 calls and linguistics, and an invite to attend a Cardiac Prevention Awareness Event organised by the Jewish Community Foundation. There are also opportunities for members to engage with each other on a dedicated PPP members area of the trust’s website. There is more work in progress to further support the role of the PPP including.
- Our PPP charter has been reviewed and now includes key information for our PPP members when attending trust meetings and what they can expect from us to keep them informed and supported fully as members. The reviewed PPP charter will be launched and sent to the membership early 25/26 through the PPP newsletter.
- Our PPP forum is not frequently accessed by PPP members. We will consult PPP members on how the forum can be better utilised including any changes to the layout of the forum to make it more accessible and easier to use.
- Further to a variety of requests from integrated care board (ICB) commissioners for PPP support with some of their projects and initiatives, further development training will be sourced for PPP members to enable them to confidently get involved with high level projects and meetings.
A trust celebration event is being planned for the Autumn of 2025 where PPP members will be invited and recognised for their contribution.
Patient, public and community engagement
Whilst patient surveys provide us with a real insight into the care and treatment that patients have received, another method used to gain qualitative feedback is by engagement with community and patient groups within our region. Our focus has been to reaffirm the basics of what we offer across each of our three main service lines and to explore any misconceptions and/or barriers to access. We have also used these valuable face-to-face opportunities to offer our communities information about self-care, winter health messaging and offer service-based activities to elicit their understanding and experience of care.
During 24/25 we attended nine virtual engagement events, and 22 face-to-face engagement sessions which were attended by the trust as principal speakers, advisors or facilitators. These events included the Kashmir Youth Project, Wirral Multicultural Organisation, Greater Manchester Faith forum, Wai Yin society and the Chinese Wellbeing group in Liverpool.
Further support is provided to our patient groups upon request, for example supporting cardiopulmonary resuscitation (CPR) training. Examples of the groups we have supported include the Liverpool Chinese Students and Scholars Association (LCSSA) and the Chinese Wellbeing group in Liverpool. This work will continue with the British Islamic Medical Association (BIMA) and the Lancashire Council of Mosques during 25/26.
In addition to this we have also been able to support 29 high attendance events in 24/25. Examples include PRIDE, university freshers events, Greater Manchester Ethnic Communities Network Event, a Cardiac Prevention Event within the Jewish community and the Liverpool Chinese Students and Scholars Association (LCSSA) Spring Festival Gala. Our engagement with the Jewish and Chinese community has considerably increased this year due to our continued focus and support.
Targeted work with young people, including oversees students, provides an opportunity to offer information about accessing NHS services. In addition, it has provided individuals with an opportunity to explore volunteering and career opportunities within the ambulance service or the wider NHS.
Protected characteristics
The Equality Act 2010 identifies nine protected characteristics cited as: age, disability, gender reassignment, race, religion or belief, sex, sexual orientation, marriage and civil partnership, and pregnancy and maternity. During 24/25 we have engaged with people who have identified as having a protected characteristic.
The graph below shows the number of people we have engaged with who identify as having a protected characteristic.

Quality improvement initiatives with underrepresented groups
Our Patient Inclusion team has established a task and finish group to ensure under-represented voices are included in decision-making.
As part of this work, we’ve begun engaging with Chinese and Jewish communities in the North West through focus groups. These sessions aim to understand their experiences, expectations, and any barriers to accessing our services. Feedback will help identify gaps in representation and drive meaningful improvements.
Ambulance awareness day events
Over the past year, we successfully delivered five county-based face-to-face community awareness events. Our Greater Manchester event, held alongside the trust’s annual general meeting, featured information stands from NHS 111, PES, PTS, and corporate staff, as well as CPR training sessions. It attracted 203 attendees – 66% from ethnic minority backgrounds, 15% from the Chinese community, and 40% aged 16 – 24.
In Cumbria, Lancashire, Cheshire, and Merseyside, Ambulance Awareness days used interactive tabletop exercises and themed speakers to raise awareness, gather feedback, and discuss PES, PTS, and NHS 111 services. These activities helped identify what’s working well and where improvements are needed. Based on feedback, we developed a snapshot of service improvements and an accessible summary document, shared with attendees in August 2024 and published on our websites. Some activities also supported Winter demand planning – for example, NHS 111 tables addressed common concerns like repeat prescriptions during public holidays, supported by useful giveaways and leaflets.
We select event venues in areas frequently used by local communities, often where health outcomes are poorer. This has helped us reach groups that are typically harder to engage. Attendee demographics are shown in figure 7. Feedback summaries and planned improvements are shared with attendees and community groups, and this approach will continue into 25/26 as we review future event locations.
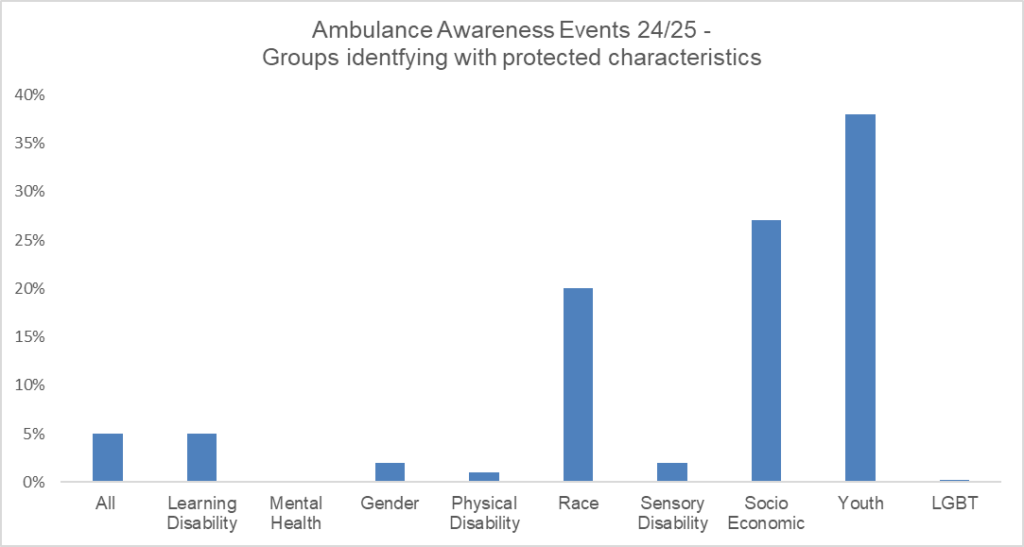
Examples of feedback themes received from events include:
- Staff very friendly, enjoyed the CPR training and HART stand
- Very good event, very satisfied with the stalls and activities on offer
- Good development for any PPP member, great opportunity for the community, excellent practical exercises
- NWAS dyslexia support for existing staff and recruitment
- Good information on how to deal with mental health calls
- Helpful information on how to support patients whose first language is not English, including basic British Sign Language (BSL) training available to operational staff
- Information on how to find a patient from a mobile number calling 999
Filmed patient and staff stories
Filmed patient and staff stories remain a powerful way to highlight real experiences and share learning. These are shared bi-monthly with the NWAS Board of Directors and Quality and Performance Committee, included in staff training, and featured in education and awareness campaigns.
In 24/25, patient stories covered topics such as STEMI response times, heart condition pain awareness, and winter pressures. Staff stories included the HALO Project (redefining the ambulance liaison officer role), the Care Home Engagement Project, and the Aspirer welfare initiative.
Patients’ experience recommendations and improvements
Feedback gathered through patient engagement is used to shape improvement recommendations. Learning dashboards are produced for PTS improvement ambassadors to share insights and support co-designed service changes. In 25/26, this approach will expand to include PES and NHS 111 services.
Some of our recommendations and improvements include:
- Feedback from the Chinese community highlighted concerns around service awareness and language barriers. In response, we translated 999 and PTS leaflets into Cantonese and Mandarin and are producing a film showing how we support communication in patients’ spoken languages. This will form part of a shared patient story within the trust.
- Feedback from the Lancashire School of Mosques emphasized the importance of ambulance staff wearing shoe covers in Muslim homes. In response, we shared guidance in our staff bulletin, intranet ‘You Said, We Did’ section, monthly newsletter, and directly with the School of Mosques.
- At a community event, feedback highlighted the need for greater staff awareness when entering homes. In response, we launched the NWAS Religion, Belief and Culture Card, offering guidance on common first languages, cultural norms around physical contact, and end-of-life customs to support more respectful and informed care.
- Feedback from community engagement highlighted growing interest in CPR training and the need for better understanding of DNACPR (do not attempt Cardio-Pulmonary Resuscitation). We will respond to CPR training requests and incorporate DNACPR awareness into future community engagement plans.
- In 24/25, our Ambulance Awareness day events were updated based on attendee feedback to include a knife incident scenario and mental health talks. We’ll continue sharing county-specific mental health support information through our community info burst newsletters.
- We collaborated with the Research and Development and Widening Access teams to introduce 3D virtual reality ambulance headsets at our Ambulance Awareness day events. These were especially popular with young attendees. We plan to continue this partnership to offer the headsets at future events.
- Patient Engagement colleagues to undertake facilitator training to support with leading on conversations and group discussions at external events.
- Promoting our attendance at community engagement events using scheduled social media channels to highlight where patients and groups can meet us.
- Targeted attendance with schools and colleges ensured all our Ambulance Awareness day events were well attended by a young generation pursuing a career in the ambulance service. We will continue to build on this with profiling job roles, routes to employment and volunteering within the ambulance service at our community events during 25/26.
- Our PTS Level 2 learning dashboard enables the sharing of patient feedback, promoting best practice and boosting staff morale. During 25/26, we will ensure that PTS managers highlight this data on all NWAS stations that have visual display screens.
- Increased survey feedback from underrepresented groups to ensure the development of demographic feedback into our digital platforms – this will be supported by additional outreach to increase survey feedback from Black, Asian, and Minority Ethnic (BAME) communities
- Feedback from our deaf communities who continue to share concerns and barriers to accessing our services. As a result, we will produce an ‘Insight App’ film for operational staff awareness with using language and BSL interpreters at patient side. We will also feature the Blue Light Academy basic sign language training as part of this work.
- Supporting frontline staff awareness with the various accessibility tools available, we shared a staff bulletin signposting this information on our trust intranet Green Room. We will continue to review and update this information annually.
- Easy read formats of our service information provided to Ambulance Awareness day attendees with learning difficulties. Further work will include an easy-read production of the event evaluation form. Alternative format is ensured in our regular communications with our communities in all publications including monthly info-bursts and PPP Weekly Round ups.
- A health literacy improvement project to create new, accessible information for patient transport service users.
Complaints
Complaint management
Complaints are managed by the Patient Advice and Liaison Service (PALS) and Resolution team, who ensure open and honest investigations which are aligned with relevant legislation and the Model Complaint Handling Procedure as outlined by the Parliamentary and Health Service Ombudsman (PHSO). Our goal is to achieve satisfactory resolution for complainants, while maintaining compliance with best practices.
NWAS remains steadfast in its commitment to delivering a high-quality and patient-centred complaint experience. We recognise the importance of all concerns, complaints and feedback as essential tools for continuous improvement. Insights from patients, their families, and service users allows us to assess our practices, identify areas for enhancement, and implement necessary changes at both individual and system-wide levels.
The PALS and Resolution team ensure that individuals who raise concerns feel heard and that their complaints are addressed effectively. In 24/25 we saw specific focus on evolving our responses to complaints, making sure that letters and communications are patient centred, and always demonstrate empathy and compassion. The PALS and Resolution team continue to address complaints with fairness and transparency with the end goal being to improve a patients experience and drive service improvement.
The NWAS Board of Directors receive information about complaints through several structured reporting groups and committees. This framework enables NWAS to ensure that patient feedback is not only acknowledged but also used constructively to highlight the patient journey and identify recurring themes or trends in complaints. These insights are addressed with appropriate actions, providing assurance that improvements are made where needed.
We understand that raising a complaint with a large organisation like NWAS can feel overwhelming and is often perceived as a negative experience. However, the PALS and Resolution team is committed to ensuring that this isn’t the case. Recently, a patient shared feedback, with a manager, expressing how supported and reassured she felt by the team when raising her complaint.
“Thank you for your support and understanding of my issue. I would like to thank you both for your kindness and understanding in previous communications! It gives me faith that we are listened to when things go wrong! Thank you so much again”
Achievements during 24/25
The PALS and Resolution team has stabilised both their resilience and their performance over the past year. The team has worked hard on securing processes in line with legislation and PHSO (Parliamentary Health Service Ombudsman) guidance and training opportunities have informed continued professional development. This has benefited the quality of complaint handling.
To build on this, system improvements were also identified and modifications required to the Datix Cloud IQ (DCIQ) complaint module. This has now been completed, and the start of 2025 introduces new complaint categories and learning outcomes to help identify themes of complaints and learning. This is beneficial for users of the system, the analysis of data reported into the system and of course, our patients and the service improvements we can recommend as a result.
Additional work has been carried out to capture the protected characteristics of patients who raise complaints, allowing for more meaningful analysis to support wider outreach initiatives. This has involved close collaboration with the Patient Engagement team in their ongoing efforts to connect with all communities served by NWAS. The PALS and Resolution team is committed to accessibility for all, making use of services like ‘Language Line’ when needed and adapting forms and correspondence into ‘easy read’ formats. Discussing and addressing communication needs is now a routine part of the complaint process, ensuring that individual’s requirements are understood and met from the outset.
Complaint figures
Last year 2,277 complaints were raised with us and 89% of these were recorded as ‘low complexity’ complaints, which were managed by the Patient Advice and Liaison (PALS) team. The PALS team guide appropriate and empathetic apologies within an everyday conversation, as guided by the PHSO’s standards.
The three most common themes of complaints received related to:
- Care and treatment
- Delays
- Call handling
Care and treatment
The table below shows the number of complaints about Care and Treatment managed at each level of complexity.
| High | Medium | Low | Total |
| 20 | 113 | 781 | 914 |
A full breakdown of the sub-categories shows the specific genre of treatment complaints, raised with NWAS.
| Sub-type of complaint | Number of complaints |
| Professional standards (conduct) | 619 |
| Disposition | 165 |
| General | 79 |
| Clinical treatment | 42 |
| Equality | 6 |
| Assessment | 3 |
| Total | 914 |
The complaints regarding care and treatment by service line and area, may vary from total number provided above, as a singular complaint, may involve multiple service lines.
| Service line | Number of complaints |
| Patient transport service | 268 |
| Greater Manchester, paramedic emergency service (PES) | 199 |
| Cheshire and Merseyside (PES) | 181 |
| Cumbria and Lancashire (PES) | 164 |
| NHS 111 | 113 |
| Emergency operations centre | 48 |
Delays
In the last year, 734 of the complaints included concerns about a delay in service. Below, outlines the complexity level assigned to each complaint.
| High complexity | Medium complexity | Low complexity | Total |
| 9 | 33 | 692 | 734 |
| NWAS service line | Number of complaints |
| Paramedic Emergency Service (PES) | 585 |
| Patient Transport Service (PTS) | 149 |
Call Handling
Concerns about an aspect of the call handling part of a patient’s journey featured in 364 of the complaints.
| High | Medium | Low | Total |
| 7 | 33 | 324 | 364 |
| NWAS service line | Number of complaints |
| NHS 111 | 166 |
| Paramedic Emergency Service (PES) | 155 |
| Patient Transport Service (PTS) | 43 |
Complaint outcomes
We closed 2,242 complaints in 24/25 with 86% of all complaints closed within local Service Line Agreement. This is an improvement on the 85% closure within local service line agreement achieved in 23/24.
We closed 2,242 complaints in 24/25 with an improved performance in closure rate with 86% of all complaints closed within local service line agreement timescales.
| Complaint Outcome | Complaint Level | Total | |
| Upheld | High | 15 | 622 |
| Medium | 53 | ||
| Low | 554 | ||
| Not Upheld | High | 11 | 928 |
| Medium | 88 | ||
| Low | 829 | ||
| Partly Upheld | High | 5 | 692 |
| Medium | 57 | ||
| Low | 630 | ||
Parliamentary and Health Service Ombudsman (PHSO)
In 24/25, NWAS received 10 notifications from the Parliamentary and Health Service Ombudsman (PHSO) regarding complaints submitted for independent review.
- Three cases were closed following an initial assessment, with no failings found on the part of NWAS.
- Two cases were resolved through mediation or further local review and subsequently closed.
- One case was not upheld, with the PHSO identifying no failings by NWAS.
- One case was partly upheld, resulting in a recommendation for further apologies to be offered to the complainant.
Three cases remain open as we move into 25/26 and are currently under detailed investigation by the PHSO.
Patient Safety Incident Response Framework (PSIRF)
PSIRF promotes a proportionate approach to responding to patient safety incidents by ensuring resources allocated to learning are balanced with those needed to deliver improvements. The principles of PSIRF are to:
- Advocate a co-ordinated and data-driven approach to patient safety incident responses, that prioritises compassionate engagement with those affected by patient safety incidents.
- Embed the patient safety incident response within a wider system of improvement and prompt significant cultural shifts towards systematic patient safety management.
NWAS Executive Leadership Committee, Quality and Performance Committee, and the Board of Directors identified local priority areas which commenced from October 2023. These remained in place during 24/25 and are:
- Prevention of deterioration to critically unwell patients with contributing harm.
- Errors in 999 and 111 call handling which led to a delay with contributing harm.
- Face-to-face or telephone assessment which is managed down an incorrect pathway contributing to harm.
This year has seen the first full 12 months of the PSIRF, during which we have identified and commissioned 18 level 1 learning responses otherwise known as Patient Safety Incident Investigations (PSIIs). In these we seek to use a systems engineering based approach to consider the opportunities where improvements can be made to help our people to do the right thing, every time. This is a change to root cause analysis used in the serious incident framework and asks the patient safety event Investigators to consider the complexity of the work and its interactions, assumptions and ‘work as done’ rather than ‘work as imagined or prescribed’. This approach encourages open discussion as to why events took place in the manner they did and relies on an appreciative inquiry approach to problem identification and solving. We have found this innovative approach to working with our people and teams encourages an openness and has helped us to learn how we can best support our people who work in this demanding environment.
The first 12 months of PSIRF has allowed us to undertake some improvements to the internal governance processes supporting the framework.
- We have worked closely with patients and families to improve the language used in the PSII reports to remove acronyms and include accessible language explanations for complex clinical interventions.
- With the families and patients’ agreement we include photographs and biographies of the patient involved in the patient safety event, to keep the patient at the very heart of the review. In addition, we have developed patient stories in conjunction with patients and families which are presented both internally and externally to support improvement
- Our engagement leads act as advocates for the patient and their families throughout the process. The leads bring forward any queries patients and families may have, support the interpretation and sharing of draft reports and are the main point of contact for progress updates. The engagement leads are available to support the families with translation services and all manner of things pertinent to the PSII including sign posting to well-being agencies and helplines.
- We have improved our internal processes of PSII management to include a multi-disciplinary team case conference within seven days of PSII commission, and a further case conference at day 30 to ensure all elements are on track.
- An external independent audit of PSIRF, its implementation and current governance processes was conducted. The review concluded in March 2025 and NWAS was assessed as providing substantial assurance. Furthermore, the auditors summarised ‘there is a good system of internal control designed to meet the system objectives, and that controls are generally being applied consistently’ which is testament to the team and stakeholders who are responsible for delivering PSIRF on behalf of the organisation.
- There have also been ongoing improvement programmes linked to PSIRF and the findings from patient safety incident Investigations including improvements to call handling and dispatch, mental health and medicines management.
- We have also embedded a regional clinical learning and improvement group, where learning from the Patient Safety Incident Response Framework is shared, and safety improvement actions overseen.
Patient safety events
During the last financial year 8,479 patient safety events were reported into our incident management system. Patient safety events are assessed in terms of the actual impact of the incident on the patient. The table below described the levels of harm confirmed for 8,085 patient safety events. The level of harm for 394 patients remains unconfirmed at the time of writing.
| Confirmed level of harm 24/25 | Q1 | Q2 | Q3 | Q4 | Total |
| No physical harm | 1563 | 1664 | 2225 | 1383 | 6835 |
| No psychological harm | 58 | 61 | 51 | 38 | 208 |
| Low physical harm | 199 | 172 | 165 | 83 | 619 |
| Low psychological harm | 24 | 27 | 24 | 11 | 86 |
| Moderate physical harm | 41 | 59 | 49 | 37 | 186 |
| Moderate psychological harm | 4 | 5 | 2 | 1 | 12 |
| Severe physical harm | 9 | 19 | 7 | 11 | 46 |
| Fatal | 17 | 24 | 28 | 24 | 93 |
| Total | 1915 | 2031 | 2551 | 1588 | 8085 |
Patient safety event categories
Four patient safety event categories account for 68% of all patient safety events reported during 24/25. These are:
- Care and treatment: 2,244 (26.5% of the total number of patient safety events in year)
- Call handling: 1,408 (16.6% of the total number of patient safety events in year)
- External organisation enquiry: 1,153 (13.6% of the total number of patient safety events in year)
- Delays: 969 (11.4% of the total number of patient safety events in year).
During 24/25, we received 1,247 external incidents from other NHS providers. We also raised a further 963 patient safety events to other organisations requesting a response to patient safety incidents.
| Organisation involvement | Q1 | Q2 | Q3 | Q4 | Total |
| External In – incident received from another organisation | 10 | 149 | 802 | 286 | 1247 |
| External out- NWAS raising an incident with another organisation | 5 | 95 | 410 | 453 | 963 |
| Total | 15 | 244 | 1212 | 739 | 2210 |
A collaborative review of the patient safety incidents, complaints, concerns and issues has taken place during the latter part of 24/25 and new local PSIRF priorities have been identified and are due to be approved for the year ahead. This information will be disseminated with internal and external stakeholders, with safety improvement plans developed linked to our strategic aims.
Incidents (staff and trust)
During the last financial year, 8,465 staff and trust incidents were reported. Our incidents are risk scored using the trust’s risk matrix to assess the consequence.
| Risk Score | Value |
| 1 | 2,583 |
| 2 | 4,569 |
| 3 | 1,258 |
| 4 | 53 |
| 5 | 2 |
| Total | 8,465 |
The most common incident categories were violence and aggression (1,952), medicines: controlled drugs (658), road traffic incident with vehicle (629), road traffic incident with object (521) and accident and injuries (443).
During 24/25, we received 208 external incidents from other NHS providers.
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 24/25 | 67 | 49 | 59 | 33 | 208 |
In addition to the external incidents coming into the trust, we raise incidents to external agencies and health and social care organisations. During 24/25, we sent 143 external incidents to other organisations requesting to a response to staff and trust incidents.
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 24/25 | 35 | 16 | 50 | 42 | 143 |
Clinical Safety Plan (CSP)
Timely action and resource management are crucial to prevent patient care compromise during high demand periods and the NWAS Clinical Safety Plan (CSP) details how safe service delivery is managed amidst varying demand levels. It focuses on proactive measures to manage clinical risks and maintain public confidence. The CSP maintains consistent and safe service delivery, particularly during demand surges and response deterioration, and addresses high-risk situations.
The CSP dynamically responds to service pressures while ensuring safe and clinically appropriate care, aligning with NHS England standards. A clear delegation scheme coordinates responses to challenges, with specific roles for the Regional Operations coordination Centre Tactical Commander and others. Detailed communication protocols ensure transparency during high demand.
The CSP includes a risk assessment framework monitoring demand, resource availability, and incident cycle times to proactively manage risks. Documentation of decisions supports accountability and future reference. Specific actions, triggers for escalation, and a risk assessment log support implementation.
Building on previous years’ experiences, CSP actions have been automated and delegated to ROCC tactical commanders, enabling rapid adaptation and management of clinical risk. Further measures have been introduced that allow NWAS to appropriately validate higher priority outcomes proportionately if response times deteriorate.
Winter safety review
Each year, we undertake a review of safety over the winter to identify themes and trends and opportunities for improvement. We have undertaken a review in December 2024 and January 2025 analysing patient events resulting in harm. This has identified the following themes:
- Category two calls continue to make up the highest percentage of severe or fatal harm patient events
- The predominant theme in severe or fatal harm patient events continue to relate to delays
- The age range most affected in the patient safety events reviewed is 65-84
- Like previous years, patients who are receiving palliative or end of life care, and patients with frailty or other long-term conditions are predominantly affected in the harm related patient safety events reviewed.
Freedom to speak up
In addition to speaking up through leadership teams and normal workforce processes, we have established well embedded additional speaking up processes to create a culture of safety. We continue to foster a culture where our people feel safe to speak up and raise concerns. This in turn allows us to provide highly effective care where we learn when things might not go well. Our team of Freedom to Speak Up (FTSU) guardians have this year seen a reduction of 21.4% in the number of concerns raised (121 from 154 in 23/24).
Ambulance services, in line with other blue light services, have come under increased scrutiny from the national media along with NHS England. The Thirlwall Inquiry prompted a comprehensive review of all NHS speaking up arrangements.
We provide a number of ways to encourage speaking up processes, such as the Datix cloud IQ (DCIQ) platform (our incident reporting process), staff forums, Freedom to Speak Up guardians, staff Facebook pages and appraisals, along with directly with leadership teams. These channels enable our staff to voice concerns about their wellbeing, the care they provide or cultural issues.
This year has seen 121 concerns raised with the FTSU guardians, categorised into themes according to the National Guardian’s Office (NGO) returns.
| Themes | Percentage | Number |
| Inappropriate attitude and behaviours | 61.2% | 74 |
| Patient safety | 15.7% | 19 |
| Bullying and harassment | 13.2% | 16 |
| Worker safety | 6.6% | 8 |
| Fraud | 0.8% | 1 |
| Detriment | 2.5% | 3 |
The proportion of patient safety concerns has decreased. We have focused on the many ways in which staff can raise any concerns from informal/formal discussions with local mangers and leaders through to formal paths such as Grievance/Dignity at Work process and safety concerns raised through our Incident reporting system.
Through a formal leadership development program, leaders are equipped to make themselves ‘open’ to discussion and actively listen to staff concerns. This enables leaders to negotiate positive outcomes that meet the staff needs and addresses their concerns whilst also considering impacts on all staff, patients and the organisation.
We have instigated several new processes to ensure we deal with concerns in a consistent way, ensuring an impartial view which supports both staff and managers to resolve concerns using learning. This reflects in the feedback we have received from staff and managers who have been involved with FTSU guardians.
What our staff tell us
Staff member: “I have placed a ‘no’ under the problem being resolved as it hasn’t yet, however fully recognize that the processes in place will eventually address the matter. My experience is that FTSU appears to be effective and is a valuable tool to the organisation”
Staff member: “No concerns for areas to improve on. The issue I raised was escalated quickly to the ICC senior leadership team with a resolution reached in under a month.”
Staff member: “In my case, the process worked very well. The communication maintained with all parties (including the FTSU team within themselves) was a huge strong point”
New freedom to speak up guardian: “As a new FTSU Guardian with NWAS, and one of three, we continue to embed the two recommendations the National Guardian’s Office report ‘Listening to Workers’ made to ambulance trusts. Our policy continues to reflect the NHS policy on ‘speaking up’ and is compliant with current requirements. We have seen a decrease in the number of concerns. As a staff member who has held numerous posts within NWAS including senior management my passion has always been about nurturing a supportive, safe culture. This is gaining strong traction in many areas of NWAS. This fosters confidence and trust that allows staff to raise concerns locally, be heard, and concerns address at source, which is the best outcome for all. In this year’s NHS staff survey 61% felt safe in to speak up about anything that concerns them in the organisation. This is 6% above the NHS average and equal top performing in the ambulance sector.”
Support and guidance from the non-executive lead for FTSU has again this year been invaluable to ensure we address any concerns raised by external providers.
Staff safety (violence prevention, reduction, and security)
Violence and aggression against ambulance workers has been on the increase both locally and nationally year on year. In 23/24 there was the highest recorded number of incidents reported. A Violence Prevention and Reduction team was recruited in 2024, to primarily focus on staff safety, staff support and a public health approach in collaboration with partner agencies to prevent and reduce violence and aggression. Specific pieces of work have been initiated this year which look at reducing staff being assaulted and preventing repeat offending of abuse to our integrated contact centre staff.
All staff now have a Violence Prevention Reduction Specialist Practitioner assigned to them when they make a report of violence and aggression. This is to ensure that all staff get the right level of support post incident, that all incidents are addressed and that perpetrators are effectively managed and dealt with through partnership working and information sharing.
The Violence Prevention and Reduction team map trends and patterns of behaviour through data collection to identify and implement interventions that both aim to prevent the offender from reoffending and support the staff members involved. This ensures that that all individuals involved are given appropriate support and are made aware of the outcome after an incident has occurred. Through accurate data mapping, intervention, partner agency working, training and education for our staff, and public engagement the Violence Prevention Reduction ` is seeing positive outcomes in both prevention and reduction.
Other specific initiatives this year includes:
- BBC media campaign on the increase in violence and aggression against ambulance workers.
- Partner initiatives with police/councils/education/violence reduction unit and other health care providers.
- Improved mandatory training that is designed through current data collection of incidents to make it bespoke to the incidents staff are facing.
- Education and awareness events for staff.
- Collaborative working with staff networks and trade unions.
- New working groups set up and established to focus on tackling violence and aggression
- Increase in the use of body worn video cameras by staff.
- Trauma informed/public health interventions – understanding the cause of the violent behaviour and addressing the causes through partnership working and education.
Health, safety and security and fire
We are committed to providing a safe environment for our people and others who are involved, or affected by the activities of the trust, so far as is reasonably practicable, in accordance with the Health and Safety at Work Act 1974 and associated legislation. Every employee has a personal responsibility for health and safety, including following policies and procedure to keep themselves, their colleagues and patients safe throughout the course of their duties. Our partnership with health and safety trade union colleagues remains strong and they are full members of our Health, Safety, Security and Fire group and work with service lines on local health, safety, security and fire management.
Reporting of Injuries, diseases and dangerous occurrences regulations (RIDDOR) 2013
During the last financial year 126 incidents were reported to the Health and Safety Executive (HSE) under the RIDDOR regulations.
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 24/25 | 29 | 33 | 35 | 37 | 134 |
Safeguarding vulnerable children and adults
The Safeguarding team has a statutory function within North West Ambulance Service and liaises with both internal and external multi-agency partners in respect of statutory safeguarding reviews (domestic abuse related death reviews, safeguarding adult reviews and child safeguarding practice reviews) and local authority designated officer (LADO) referrals in cases where a staff member may be considered a risk to children. It is also the responsibility of the head of safeguarding to report ‘Prevent counter terrorism data’ to NHS England.
The Safeguarding team works across the trust and with partner agencies, including commissioners, social care, police and health partners, to review and improve the quality of the safeguarding service provided by NWAS staff, ensuring that our employees and volunteers have the appropriate knowledge and skills to discharge their safeguarding function. NWAS, via the head of safeguarding, provides assurance to the Lancashire and South Cumbria ICB via the designated professionals for safeguarding, that the service is well led and managed and discharges its statutory responsibility in line with legal obligations.
Safeguarding processes are continually reviewed, and the Safeguarding team liaises both locally and nationally, using statutory reviews, audit, legislative updates and general information sharing to highlight updates, hot topics and emerging issues. These inform training and service development within the organisation. The Safeguarding team at NWAS regularly shares key information with staff, both internally and across social media platforms.
Safeguarding referrals
NWAS makes safeguarding referrals to 27 local authorities within the geographical footprint. Referrals are made electronically via our support centre in Carlisle to the appropriate local authority. During 24/25, NWAS made 39,561 safeguarding and early help referrals, as shown in the figure below. NWAS early help referrals are predominantly for adults who may benefit from an assessment of needs. The number of referrals rejected by local authorities is less than 2%, indicating that the safeguarding information we share is of a high quality.
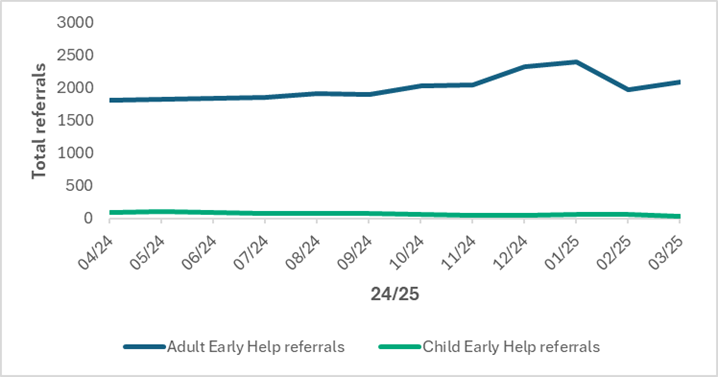
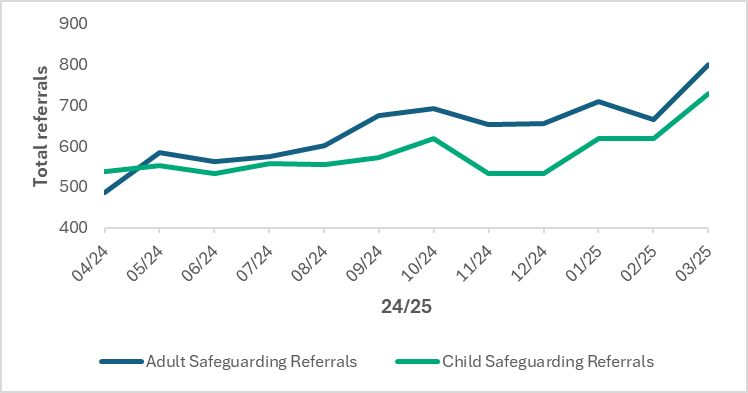
Safeguarding training
The Intercollegiate Documents for Adults (August 2018) and Children (January 2019), published by the Royal College of Nursing, set out minimum safeguarding training requirements for health staff. NWAS is committed to ensuring that high quality safeguarding practices exists across all business areas of the organisation, with training essential to achieve this. During 24/25, the Safeguarding team has worked with the Learning and Development team to align all new roles with the appropriate level of safeguarding training and trust-wide training compliance has been maintained throughout the year.
Key safeguarding achievements during 24/25
- An outcome of ‘Substantial Assurance’ was achieved following a safeguarding audit by Mersey Internal Audit Agency (MIAA) in December 2024.
- Restructure within the Safeguarding team has enhanced cross working and sharing of expertise between safeguarding and mental health staff.
- Development and implementation of a safeguarding dashboard.
- Continued engagement with integrated care boards to streamline assurance requirements and to provide a conduit to safeguarding boards/partnership boards.
- Continued development of easily accessible safeguarding resources for our workforce.
Improving services for people with a learning disability
Following our trust’s successful NHS England bid in 2022 to develop a new Learning Disability and Autism (LD&A) plan, and to add a dedicated specialist role to lead on the work, quality improvement projects have continued to be progressed.
The NHS Long Term Plan listed learning disability as one of its healthcare improvement priorities, recommending a system-wide collaborative approach. Our plan reflects compliance with this, as well the national Learning Disability Improvement Standards, National Mortality review learning, NICE guidelines and current Care Quality Commission (CQC) regulation of mandatory training and awareness to all healthcare sectors. This work also supports the Association of Ambulance Chief Executive’s (AACE) current agenda to reduce health inequalities following a national consensus with major healthcare organisations.
In 24/25 we have:
- Continued to cultivate valuable feedback from our patients and our specialist partners to gain recommendations and to inform good practice.
- Interrogated appropriate cases of complaint, serious incident reporting and mortality reviews to inform thematic analysis and further learning. This supports patient safety projects on the back of Patient Safety Incident Response Framework (PSIRF) investigations.
- Sustained collection of direct feedback from our neurodiverse staff to gauge their opinions on our practice, providing rich insight.
- Sustained near 90% compliance with the first element of the respective mandatory training across service lines, meeting the regulatory requirement from the Care Quality Commission.
- Updated an internal enhanced sector specific e-learning module on the LD&A subject matter based on the learning from the co-produced strategic plan which is available to all staff.
- Continued the membership of the Sunflower Scheme and included hidden disability awareness subject in staff inductions.
- Continued enhanced sensory provision as standard in new ambulance vehicles in the fleet. This supports the quality of assessment for patients with sensory needs. Further collaboration between the mental health and digital innovation teams will support the SMART vehicle project.
- Started the development of a ‘Care Interaction Tool’ digital application for staff iPads that aims to enhance neurodivergent patient experience, aid our assessment and decision making for patients.
- Introduced an official cross service line ‘Neurodiversity Champion’ network who can provide peer support through lived experience to colleagues who may be facing challenges with neurodivergent conditions.
- Sustained representation at LD&A community and partner engagement events in collaboration with the Widening Access team. There is ongoing engagement with our Patient Public Panel, regional LD Partnership Boards, the North West Learning Disability (LD) Operational Delivery Network and our Disability Network; this ensures we continue to hear the voice of our patients and partners.
- Continued to engage with hospital and community learning and development teams, supporting pro-active organisation of enhanced pathways/flags and personalised care for complexed patients. Complex patient markers and hospital passports can also be made available on the internal Cleric platform allowing access by our senior clinicians.
- Continued closer feedback relationships with ICB learning from life and death reviews (LeDeR) has improved consistency and accuracy of reporting. There is ongoing closer engagement with ICBs to share learning and identify patient safety themes.
Mental health services
Our Mental Health team work at strategic level with system partners to deliver on the aspirations of the NHS Long term Plan (2019) and to improve the safety, effectiveness, experience, and outcomes for patients contacting us with a mental health need. An overview of the progress and achievements during 24/25 is summarised below.
Mental health practitioners in our integrated contact centres
The model varies across our footprint:
In Greater Manchester, mental health practitioners employed by the mental health trust have been providing support for 12 hours per day, seven days per week. Confirmation of funding has now been secured and the NWAS Mental Health team is working with Greater Manchester Integrated Care Board and trust partners to develop the longer-term 24/7 model which will be implemented by October 2025.
In Lancashire and South Cumbria, mental health practitioners continue to triage mental health calls 24/7 via our integrated contact centre in Preston. On-going engagement continues with the integrated care board to secure commitment for the continuation of this model.
We are also working with Cheshire and Mersey Integrated Care Board and with mental health partners to agree a model for the management of Category 3-5 mental health calls, with the aim of ensuring that patients in mental health crisis are supported by the most appropriate service to meet their needs.
Implementation of the NHS 111 ‘Option 2’ in April 2024, provides a single point of access for patients who present with a mental health crisis. Evaluation work will continue with system partners, NHS England and Integrated Care Boards throughout 25/26 to ensure the service remains timely and patient focused.
Mental health response vehicles
Throughout 24/25, the NWAS Mental Health team have continued to work collaboratively with integrated care boards, NHS England and partner trusts to implement the Mental Health Response Vehicle Model. There are now six vehicles in operation: four in Cheshire and Merseyside (Warrington, Bebington, Northwich and Toxteth) and two in Greater Manchester (Salford and Oldham). In collaboration with partners across the region, NWAS has undertaken an evaluation of the model to identify outcomes and learning which will inform longer-term planning.
Mental health training and education
The introduction of a mental health development Practitioner role has enabled additional resilience within the team to support with the development of a suite of training in relation to undertaking a mental state examination and application of the Mental Capacity Act (2005) to practice.
Patient safety
Collaborative working with the NWAS Patient Safety Incident Response Framework (PSIRF) team has seen oversight by the NWAS Mental Health team increasingly embedded within patient safety processes. The team has access to all mental health-related patient safety events and are involved in each aspect of the process from initial event reporting, through to attendance at the Complex Case Review Group (CCRG) and Patient Safety Event Committee (PSEC). Monthly meetings with our legal team also continue to highlight new or emerging risks that require an appropriate learning response.
Right care, right person (RCRP)
This approach was designed to ensure that people of all ages, who have health and/or social care needs, are responded to by the right person, with the right skills, training and experience to best meet their needs. RCRP has now been introduced by police forces within the NWAS geographical footprint. The Mental Health team, in collaboration with our integrated contact centres, have developed numerous partnership agreements, memorandums of understanding and procedures to mitigate any potential adverse impacts of this approach.
Mental capacity
NWAS adheres to the mandatory legal framework of the Mental Capacity Act (MCA) 2005 as outlined in our trust policy.
During 24/25, staff undertook:
- Mental Capacity Act learning resources on the NWAS Continued Professional Development and Learning Hub.
- Ambulance Mental Health Induction module available on the electronic staff record training library.
- Mental capacity induction training for emergency medical technicians working on mental health response vehicles.
- Mental capacity refresher training as part of NWAS face-to-face mandatory training.
In terms of monitoring the use and consideration of the MCA our electronic patient record (EPR) platform incorporates mandatory fields that our clinical staff will complete when finalising a report and considerations of care surrounding capacity are pertinent. EPR data is available to NWAS audit teams.
Infection prevention and control
Infection, prevention, and control (IPC) measures are vital in protecting the health, safety, and welfare of patients and staff. The IPC Board Assurance Framework (BAF) is a framework that sets out the ten criteria from the Health and Social Care Act (2008). The IPC BAF provides assurance that policies, procedures, systems, processes, and training are in place to minimise the risk of transmission infection to service users, patients, and staff. It also identifies gaps in assurance, IPC risks and mitigations. The subheadings below, as outlined in the BAF provide information on our progress.
Systems to manage and monitor infection and risks of infection
- Assurance report from IPC Working Groups presented to the Clinical and Quality Group.
- IPC BAF and IPC Annual Report presented to board and Quality and Performance committee.
- IPC policies and procedures updated to reflect national guidance.
- All training packages are in line with the national IPC manual and updated once national guidance is revised.
- IPC public-facing webpage has been developed where information can be accessed about the IPC service.
Provide and maintain a clean environment in managed premises that facilitates the prevention and control of infections
- Cleanliness is monitored by audits conducted by Facilities and IPC team.
- All vehicles have a six-weekly deep clean. A ‘make-ready’ service is available in some areas. This is a system where ambulances are prepared by a dedicated team of staff who clean, restock and check the equipment on ambulances before the beginning and at the end of every shift.
- Policies and procedures in place to inform staff of responsibilities in relation to cleaning and decontamination.
- Station and vehicle audit results presented in an assurance report to the director of infection prevention and control at the IPC Working Group.
- A Water Safety Group meets every six months.
- Ventilation testing is carried out in line with national guidance.
- The IPC team is involved in the planning of new builds and the refurbishment of existing premises to ensure that they meet IPC requirements.
- Antibiotics are not routinely prescribed within the trust however, two antibiotics can be given in an emergency use as a one-off dose. These two antibiotics are administered under Patient Group Directions (PGD) and in line with the Joint Royal Colleges Ambulance Liaison Committee guidance (JRCALC), Joint Royal Colleges Ambulance Liaison Committee.
- Provision of on-demand information on infections for staff and patients.
- Resources available for staff disseminated regularly to staff via bulletins, social media, internal intranet, infographic posters and the IPC Working Group.
- A-Z Communicable Diseases guidance has been updated and provides links to cleaning advice.
- Individual risk assessments are carried out over the phone when booking patients onto the patient transport service. Patients are asked if they have any symptoms of infection or if they are immunocompromised to ensure that they are not placed at risk when being transported.
People at risk of developing an infection and onward transmission
- Safety stations are in place at the entrance to all trust sites with access to alcohol gel, cleaning wipes and face masks.
- Some desks within each call centre have protective screens in place for vulnerable staff/staff who wish to use these.
- Staff have access to personal protective equipment (PPE) and correct usage is taught on IPC teaching sessions.
- Regular bulletins and guidance have been published on the intranet, including updated guidance on mpox, measles and other infections.
- Face fit testing is a legal requirement for anyone who wears tight fitting respiratory protective equipment (RPE) such as a FFP3 mask as a control measure.
- Fit testers recruited in each ICB area to improve compliance with fit testing. All staff who meet the criteria are fit tested against four FFP3 masks. This is recorded on the electronic staff record (ESR). Compliance has improved significantly.
- All staff are issued with a Sundstrom hood (respiratory powered piece of equipment) on staring within the organisation for use if they fail their face fit test.
Provide or secure adequate isolation facilities
- We do not have any isolation facilities; however, staff understand precautions to take and understand the importance of informing the receiving unit to secure suitable facilities to minimise the risk of onward transmission of infection.
- Whilst we do not have direct access to a laboratory, specimens can be obtained from staff via occupational health if needed. Contact tracing has taken place for staff who have been in contact with Invasive Group A streptococcus, whooping cough, and measles. This is completed jointly by the IPC team/operations managers and staff are referred on to occupational health for further advice as necessary.
- The national IPC manual has been implemented with links to local policies and procedures. Other key policies have been reviewed and updated in line with national guidance.
Have a system in place to manage the occupational health needs and obligations of staff in relation to infection
- Staff are referred to occupational health and risk assessed by their line manager.
- Risk assessments are in place for staff who are pregnant/susceptible to infection and IPC are often consulted to contribute to these.
- Our occupational health provider has access to staff vaccination records and can provide specialist advice if a member of staff has been in contact with a patient with a communicable disease.
Maternity
During 24/25 maternity services have worked with internal and external maternity stakeholders to ensure care delivered to women using NWAS services is safe, effective, and women centred. The need to ensure that staff have the skills, confidence and resources to care for women and neonates safely, has seen the development and introduction of several interventions throughout 24/25 including:
Practical obstetric multi- professional training course (PROMPT)
Pre-hospital practical multi-professional training (PROMPT) is a multi-professional obstetric emergencies training programme that focusses on the out of hospital environment in providing maternity and newborn care.
The use of PROMPT as an effective training tool in the management of obstetric and neonatal emergencies aligns with numerous external safety reports, recommendations and, guidelines including the Ockendon report, Maternity and Newborn Safety Investigations (MNSI) and the Joint Royal Colleges Ambulance Liaison Committee (JRCALC) guidelines.
An options consideration appraisal will look at the introduction and roll out of PROMPT training across the trust has been developed during 24/25 and is currently awaiting review regarding next steps.
Pre-hospital maternity decision tool
NWAS has worked collaboratively with specialist ambulance leads from across the country to develop the pre-hospital maternity decision tool which aligns to the recommended risk tools used in maternity services. This pre-hospital maternity decision tool supports ambulance clinicians in assessing levels of need amongst pregnant/ suspected pregnant /recently pregnant women in identifying those who require a time critical assessment in an obstetric unit due to abnormal observations or red flags.
The tool was released in JRCALC in October 2025 with NWAS being the first trust to embed the tool within the electronic patient record. Next steps will be to work alongside the audit team to gather intelligent data on the impact of its introduction.
Newborn thermoregulation
After birth it is important to keep babies warm and exothermic mattresses to support thermoregulation of the newborn in the prehospital environment were introduced in 2024. A focused audit supported NWAS in identifying use cases across the organisation, with a view for a focused quality improvement project to ensure all babies born within the service receive a standardised bundle of thermoregulation care.
Maternity training collaboration
A joint training collaborative named ‘Maternity Emergencies in the Community, MEC’ saw more than 150 NWAS staff trained to deliver emergency maternity and newborn care across Cheshire and Merseyside.
This initiative provided an opportunity for NWAS clinicians to engage in learning alongside midwives at Liverpool Women’s NHS Foundation Trust, using state-of-the-art equipment to improve their clinical skills. In addition, five NWAS clinicians became trained instructors who are now able to cascade this type of training across the organisation. The success of the training was also recognised at the National Ambulance Leadership Forum with the team leads being awarded the Outstanding Service award.
Maternity and newborn safety investigations (MNSI)
NWAS has been collaborating as part of a working group undertaking a secondary analysis of maternal MNSI death investigations that included the ambulance service. The report is now finalised with key recommendations to enhance safe working practices identified and is due to be published in June 2025.
Research in maternity care
During 24/25 we have worked collaboratively on a submission to the National Institute for Health Research (NIHR) Maternity Health Inequalities Challenge, which is focused on a bespoke programme of work over the next five years to reduce inequalities in care for mothers and babies. Our consultant midwife was selected as the emerging research leader for the NIHR consortium thus strengthening NWAS’ position as a leader in the field of prehospital maternity care research.
Medicines management
Optimising medicines use and management across the service is a high priority with a Medicines team focused on this aim alongside our clinical colleagues and external partners. The vision is for the right medicines available, having the right governance to support medicines use, ensuring medicines are available for use, ensuring medicines are of a suitable quality and supporting medicines to be used safely and sustainably. This supports the Quality Strategy, and the following areas provide the workplan undertaken by the Medicines Team during 24/25:
Clinical effectiveness of medicines:
- Five new e-learning modules went live in July 2024 and a further two in February 2025 to provide training, education and assessment on medicines. Completion rates of the modules are very high.
- A new injectable medicine for seizures has been introduced for doctors working in the hospital emergency medical service (HEMS) to use.
Robust governance for medicines uses:
- A review of data has provided assurance that our ambulances are deployed with the correct medicines required.
- A review of the external ambulance service providers commissioned by NWAS for the paramedic emergency service has been undertaken to provide assurance on their medicines management.
Digital innovation and integration:
- A huge project has been completed which involved upgrading secure safes on every ambulance in NWAS. The new safes have digital locking technology that supports better governance and gives more reliable access for paramedics when some medicines are needed for patient care. Every paramedic in NWAS was issued with their own personal key to access the safes, which were configured to their own access level profile. These enhancements in security and access to medicines were implemented as part of the response to the recommendations from the Manchester Arena Inquiry.
Safe and secure handling of medicines:
- Medicines guidelines are available for clinicians to use via a nationally provided app on their electronic devices. NWAS has supported the set up and development of a new governance group to oversee the standard of these guidelines.
- An external audit of the management of controlled drugs has been undertaken and reported substantial assurance.
Medicines safety and sustainability:
- Actions have been taken to support safe administration of medicines during the intense event of a cardiac arrest and further work is underway.
Medicines safety week focused on medicines administration with videos on how to administer medicines and a ‘top tips’ poster forming part of educational tools.
Our Digital Work Programme
Our digital work programme for 24/25 is pivotal to driving our quality strategy forward and has made significant strides in advancing our Digital Strategy as part of the wider Quality Strategy plans.
To support a safety-first culture, we have:
- Enhanced our digital structure and embedded new governance arrangements. This has included investment in a robust digital framework and governance processes to ensure that solutions and systems align with the needs of the entire organisation. A trust-wide digital portfolio, supported by governance meetings, has also been developed to provide a comprehensive oversight of all digital initiatives.
- Established the Data Insights steering group with senior representatives from each directorate overseeing and prioritising reporting outputs across the trust. This has resulted in the delivery of several reporting priorities, including new dashboards for Clinical Hub, category one and two call handling, patient transport service (PTS) and public health.
- Completed the SMART Programme. This year marks the conclusion of the SMART Programme, which was designed to evaluate and drive improvements in our operations. Specifically the installation of key cabinets, station and vehicle controlled drug safes and digital wallboards for paramedic emergency service (PES), ambulance stations located within the Cumbria and Lancashire Area east sector, Morecambe Bay sector, Greater Manchester Area east sector and digital wallboards for PES ambulance stations in the Cheshire and Merseyside west sector and key cabinets for Hazardous Area Response Team (HART) sites in Manchester and Liverpool.
To support highly effective care, we have:
- Introduced a proof-of-concept point-of-care testing project. This project has been live for one year and now has funding secured for a second year of roll out and evaluation. The aim to ensure that patients receive timely and right care in the event of a suspected cardiac event not evident on an electrocardiogram (ECG).
- Continued to develop our electronic patient record (EPR). These enhancements include new tools for mental health and maternity documentation, a new falls assessment, and the development of new Ambulance Clinical Quality Indicator (ACQI) Stroke and Post- Return of Spontaneous Respiration (ROSC) care bundles. To support safe and effective patient care we have also, provided access to out-of-region EPRs for our paramedics and introduced messaging functionality for seamless communication between internal and external care teams.
- Continued to advance the PRISM Initiative. The Pan Regional Information Sharing Mechanism (PRISM) proof of concept has been evaluated and is now ready for broader piloting. This functionality integrates the North West Shared Care Records into One Response, giving frontline staff direct access to vital patient information to support safe and effective care.
- Ambulance Data Set (ADS) programme phase two completion and integrated performance reporting. Our integrated performance report has also been developed this year, with the report now shared monthly to support decision making and discussion at trust management committee meetings. The team has undertaken a significant amount of work this year on developing and flowing the ADS, a mandatory submission to NHS England to support greater understanding of ambulance activity across the sector.
To support person centred partnerships, we have:
- Focused on supporting shared decision making and releasing capacity for the analyst team. This will enable support for new areas of works, including reconciling legacy Structured Query Language (SQL) Server Reporting Services (SSRS) reports, automating regular routine reports and enhancing the triage process for ad hoc reporting requests.
- Reconciled the Power BI self-serve portal. This has streamlined existing reports to make it easier for end users to navigate, while also developing a ‘core metrics’ area, co-designed with operational colleagues. Since this development, the average number of dashboard views per week has increased from circa. 1,500 per week up to 2,500 per week. The average number of unique users has also increased from around 120 per week up to just under 200 per week.
- Progressed our Project 365 programme of work. Now in its second year, Project 365 is revolutionising our storage by migrating from on-premises servers to Microsoft 365. This supports efficient ways of working and enables effective record management for the organisation. Key milestones include:
- Migration of 30% of organisational files to SharePoint.
- Transition of all personal accounts to OneDrive.
- Removal of over a million redundant, duplicate, and obsolete records.
- Training of over 250 staff in using OneDrive, SharePoint, and Teams.
- Establishment of a Super User Network for advanced SharePoint support.
Mandatory training
Statutory and mandatory training delivery is a mix of face-to-face and eLearning for our paramedic emergency services and patient transport service staff, with other staff groups using eLearning only. The overall 24/25 year-end position is 91.17% compliance against a target of 85% and with all operational service lines exceeding the 85% target.
The core of the annual delivery is the NHS Core Skills Training Framework (CSTF) which sets out the approach to statutory and mandatory topics for NHS trusts in England. CSTF subjects are delivered across a mix of face-to-face classroom days and eLearning modules depending upon the staff group.
In addition to the CSTF requirements, we prioritised the following additional subjects in the 24/25 statutory and mandatory programmes. These were determined through collaboration across multi-disciplinary Subject Matters Experts and were informed by incident and risk:
- National level two patient safety syllabus eLearning mandated for all patient contact staff.
- The level one module was mandated for all non-clinical staff.
- Zero suicide alliance module
- Ambulance specific dementia tier 1 eLearning module (all staff)
- Ambulance vehicle fires eLearning module (all staff)
- Falls assessment (PES)
- Pocket mask (PTS)
- Maternity and newborn care (PES)
- Acute coronary syndrome with ST segment Myocardial Infarction (STEMI) (PES
NHS England statutory and mandatory training project
NHS England is leading work to optimise, rationalise and redesign statutory and mandatory training to improve staff experience, deliver better outcomes and reduce the time burden. The NHSE StatMand programme sets out key deliverables for each NHS trust.
NWAS has met all milestones set for delivery in 24/25 including:
- Alignment to latest version of Core Skills Training Framework (CSTF)
- Adopted NHS England TEL eLearning for healthcare packages
- Signed up to an interim staff movement memorandum of understanding
- Established a Mandatory Learning Oversight Group (MLOG) to oversee the outcomes for all nationally mandated training
- Produced an annual plan of mandatory learning topics
- Reviewed frequency alignment to the CSTF
Public Health
North West Ambulance Service has a focus on public health and strives for a proactive approach to improving population health within the region, going beyond reactive emergency care and ensuring our work addresses the prevention of disease and illness, contributes to health prevention and focuses upon addressing health inequalities. The executive medical director is the executive lead for public health. Under the strategic oversight of our public health lead, consultant paramedic (Medical directorate), our public health manager coordinates and oversees delivers of our public health workplan.
Our public health workplan aligns with the Quality Strategy’s objectives to develop effective collaborations with our system partners (GPs, voluntary sectors, prevention groups, etc.) and to reduce variation in patient outcomes and experience. Our focus is on identifying opportunities for our staff and volunteers to improve health and wellbeing in the population, by preventing illness and its reoccurrence and in doing so, supporting the longer-term sustainability of the NHS. Through developing and improving our data analysis we are striving for greater insight into health inequalities in the region which will enable and allow us to tailor and target our work for maximum impact.
Throughout 24/25 we have focused upon the development of our new public health workplan, driven by:
The sustainability strategy 23/26
This strategy articulated our population health commitments to improve health outcomes across our population, and our commitment to deliver positive value for the communities we serve, over and above delivery of our services.
- This Strategy articulated our population health commitments to improve health outcomes across our population, and our commitment to deliver positive value for the communities we serve, over and above delivery of our services.
The Association of Ambulance Chief Executives reducing health inequalities maturity matrix
- As part of the Association of Ambulance Chief Executives national consensus statement on the role of the ambulance sector in reducing health inequalities (published in July 2023), AACE provided an assessment tool in the form of a maturity matrix, which in alignment with national policy drivers, aimed to help ambulance trusts identifying gaps in each of four key enabling themes needed to make a difference to people who experience health inequalities. Our baseline assessment, completed in March 2024, enabled us to both benchmark ourselves at a national level and to identify gaps in our plans.
Health inequalities policy and guidance
In recent years, the national government, NHS and supporting organisations have published policy and guidance documents for Trusts to act on the reduction of health inequalities, some of these documents provide statutory actions while others are recommendations of good practice. To define the public health workplan, we considered the latest guidance, including NHS Providers’ Reducing health inequalities guide for NHS trust board members, the Long-Term Workforce Plan, and the NHS England’s statement on information on health inequalities.
The development of our public health workplan was undertaken following engagement with senior leaders, groups and committees, including the Public Health Oversight Group, and based upon outputs of this consultation our public health workplan builds on our progress achieved in the previous three years, and outlines our intentions to ensure NWAS becomes an effective system partner to improve health and wellbeing and to reduce health inequalities in our communities. Central to this are three core concepts:
- Developing solid foundations in organisational understanding of public health to enable the successful embedding of public health approaches across our working practices.
- Developing everyone’s understanding of the opportunities each of us have to make a positive impact on health inequalities and how to act on them.
- Developing our shared agreement of the top priority areas for prevention where we can make the most impact to population health across the North West.
It is envisaged that the public health workplan will directly inform and become part of the Strategy Development Programme to ensure a focus upon public health and health inequalities in all priorities across the trust, linking its objectives with the equality diversity and inclusion (EDI) objectives within the strategy as applicable. Owing to the support and collaboration with colleagues and teams from across the trust, in 24/25, we achieved our public health deliverable objectives in the annual plan.
Public Health Dashboard
In 24/25 we developed the trust’s first ever public health dashboard enabling the identification of opportunities for our staff and volunteers to improve health and wellbeing in the population. Consultation work with the Northern Ambulance Alliance network, AACE Implementation Group, and particularly Yorkshire Ambulance Service, Business Intelligence (BI) and Public Health teams helped inform our development of the population health dashboard specifications. Collaboration with the BI team enabled the design and building of our public health dashboard consisting of a series of reports on 999 calls and incidents attended, broken down by patient characteristics (age, sex, and ethnicity), and by population health data (location and deprivation index). This information will be visible to all the trust and will help develop our understanding of differences in access and outcomes by patient groups. This will also help us identify the demand from our most vulnerable groups and to proactively target interventions and developments towards reducing health inequalities.
Importantly, the data architecture developed for the public health dashboard, will enable the integration of similar population health data and reporting across other operational dashboards, helping to develop further our trust’s collective awareness of performance versus equity, which will enable conversations internally and externally about interventions to reduce variation.
Public health capacity and capability
Building capacity and capability both within the public heath team but also across the wider trust is a key enabler from which to develop our public health offer and deliver against our workplan. During 24/25, we secured a series of funding awards to support capacity and capability development:
- Through our participation in the North West Public Health Workforce Matters Regional Forum we identified and successfully gained a grant enabling the development of two learning modules; Introduction to Health Inequalities, and Introduction to Make Every Contact Count, tailored to the context of the ambulance service. Produced in collaboration between the Public Health team, the Strategy team, and Learning and Organisational Development team, these modules form the initial part of our plans to develop a trust-wide public health training aligned to the Sustainability Strategy, and the NHS’ Long Term Workforce Plan, in aiming to equip our people with the right skills and knowledge to shift care towards prevention and early intervention.
- Via the Workforce, Training and Education directorate of NHS England in the North West, we secured funding to directly support the growth of our public health workforce. This funding includes contributions towards salary costs and the apprenticeship levy and has enabled two trust colleagues to enrol on a Level 6 Public Health Practitioner Integrated Degree. Via a structured application process, colleagues from both our paramedic emergency service (PES) and our patient transport service (PTS) are undertaking the programme affording them the opportunity to both develop themselves professionally as well as developing public health knowledge and skills to apply in their own roles, contributing to improving population health.
External Collaboration
Throughout 24/25 the public health team has continued to collaborate with external system partners to actively participate in improving population health in the region.
Collaboration with the Cheshire and Merseyside Cardiovascular Disease (CVD) Prevention Board and CORE20PLUS Ambassadors scheme has supported evidence development and dissemination of the effectiveness, feasibility and acceptability of a data sharing pathway to leverage the use of ambulance data to support Primary Care partners with their secondary care prevention aims. This has the potential to improve patients’ health and wellbeing and to reduce cardiovascular acute events such as heart attacks and strokes, which have a higher occurrence in areas of higher deprivation.
This year the Public Health team completed a new pilot with a group of six GPs in Cheshire and Merseyside. This work is helping to demonstrate the potential for ambulance services to contribute meaningfully to preventative care, as well as providing evidence of effectiveness in the collaboration between the Trust, GPs, and other healthcare partners.
In 2023, in collaboration with Liverpool Heart and Chest hospital, the Public Health and the Health and Wellbeing team provided 45 cardiovascular disease health checks to staff as part of the Health and Wellbeing Festival in Liverpool. This year, through engagement with partners across the region, NWAS identified new opportunities to offer health checks at the workplace, successfully providing a total of 43 health checks in Greater Manchester. This initiative is part of a national effort from NHS England aimed at preventing hypertension, heart disease, kidney disease, diabetes, and other health issues among the workforce. Furthermore, the Health and Wellbeing team coordinated with Liverpool Liver Unit to offer staff the opportunity to receive liver scans, resulting in 40 scans being provided.
We will continue to explore and develop new partnerships and collaborations, including a focus upon academic partners to enable further evaluate and provide insight into our data surrounding health inequalities throughout 25/26. System level recognition of our work in the field of public health and the role of the ambulance service in reducing health inequalities culminated in 24/25 with our public health manager being invited onto the panel at the NHS Providers Governance Conference 2025 to discuss ‘Achieving integration at neighbourhood and place level to deliver the 10-year health plan’. Through this participation, the trust was able to articulate how the ambulance sector can play a vital role in supporting integration at a local level, including through leveraging ambulance data around specific conditions such as hypertension management and cardiovascular disease. This recognition demonstrates that the trust can play a key regional and national role in steering and shaping the ambulance sector’s contributions towards public health, something which we will build upon in 25/26.
Our improvements
Improvement in the ambulance service is about systematically refining processes, increasing safety and improving patient outcomes to ensure that services continually adapt to meet the needs of the community and deliver the best possible urgent and emergency care.
At North West Ambulance Service the Institute for Health Care’s (IHI) Model for Improvement is the core improvement approach. This is further enhanced by using theories around the psychology of change, systems thinking, measurement for improvement to understand variation and testing changes through Plan, Do, Study, Act cycles.
The Model for Improvement asks:
- what are we trying to accomplish?
- How will we know that a change is an improvement
- What change can we make that will result in an improvement?
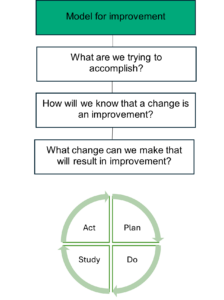
The strategic priority for the trust this year has been to undertake work on organisational culture to create a learning organisation and build improvement capability from board to frontline. Numerous research papers have highlighted that organisational commitment to developing improvement science at scale leads to better patient outcomes, increased staff engagement, and more efficient use of resources. Additionally, CQC and NHS England via NHS IMPACT highlight the importance of embedding a systematic approach to improvement. Therefore, prioritising improvement capability aligns with national strategies and regulatory expectations, making it pivotal for delivering high-quality care across NWAS.
Building improvement capacity and capability
During 24/25 work has begun to develop the organisational improvement dosing strategy and building capability offers. In short, this strategy identifies how we will build the improvement capability in our staff and how we will apply improvement to our projects and activities. The monthly Quality Improvement Network has continued invite individuals and teams to showcase improvement projects they have led or been involved with. The network is supplemented with improvement theory and introduces members to new improvement tools. The Improvement team has designed and delivered new face-to-face training offers and worked collaboratively with other teams to deliver training.
Throughout 24/25, the organisation has continued its commitment to teaching, coaching and training quality improvement skills, to ensure teams and individuals have the skills and knowledge to make measurable changes and improvements within their areas.
In 24/25 the Improvement Academy was established. Participants from the first cohort graduate in April 2025. The Improvement Academy provides substantial development in improvement science, whilst teams work on an improvement initiative that align with the NWAS trust strategy or one of the four supporting strategies. This approach supports the NHS IMPACT expectation that improvement efforts are cohesive and are focused on shared goals. With further benefit for colleagues in that it ensures that improvement is integrated into existing workstreams, rather than creating additional ‘work’.
The Improvement team building capability offers for 25/26 are being developed which will include the following:
- E-Learning: A 30-minute ESR module on basic Quality Improvement (QI) training to be completed by staff based on the Model for Improvement.
- Kickstart coaching: Structured improvement coaching for teams to work through an improvement project.
- Leading Improvement: A half day course providing focussed improvement training to teams, providing more detailed teaching on the Model for Improvement and Deming’s System of Profound Knowledge.
- Improvement Academy: An annual offer for eight teams attending nine days of classroom teaching across a nine month period, delivered through a blend of face-to-face and virtual teaching, delivered by the QI team with the inclusion of external expert speakers.
Governance of Improvement
In the past year NWAS has been further developing improvement and learning forums. The organisation has continued with the development of the Improvement Group to discuss and oversee change programmes of work and share synergies between work programmes.
The North West Improvement Academy
What is the improvement academy?
The aim of the North West Improvement Academy is to bring together expertise to support our colleagues with improvement work. We are committed to developing leaders who continuously strive for improvement in the services they provide. The Improvement Academy provides the training and tools to enable staff to deliver improvement projects that will make a genuine, sustainable difference.
We launched the first cohort of the North West Improvement Academy in September 2024. Teams attended nine days of classroom teaching across a nine month period, delivered by the NWAS improvement team along with additional input from external experts. The Academy was attended by NWAS and Blackpool Victoria Hospital teams.
The cohort learnt through workshops, learning sessions, tutorials, 1:1 coaching and project-based experience and had access to high quality resources. This programme has been built on the principles of ‘all teach all learn’, each team learns through testing their ideas and sharing these back with the whole group.
Penny Wise
Project aim: Increase the number of invoices paid, following receipt of purchase orders to 90% by September 2025 (and increase application of correct coding to 95% by the same date).
This project is important, as it will improve the productivity of the finance and procurement departments by reducing avoidable corrections and invoice processing times.
The project’s greatest achievement was to reduce the 4,387 annual transactions NWAS makes to supply drinking water machines to its sites down to 41. That’s a 99% reduction from one piece of effective streamlining!
“I’ve enjoyed working with colleagues from other teams. And seeing each of the team develop new skills and share strengths to support one another. If you want to give yourself a fresh or renewed perspective to make an improvement the improvement academy is highly recommended.”
– Andy Moody, Data Quality & Innovation Manager.
Germinator exterminators
Project aim: To ensure that 100% of NWAS staff sanitise their hands on entry to the ambulance majors entrance at Blackpool Victoria by September 2025.
Evidence shows that the single most important aspect of preventing healthcare acquired infections is effective hand hygiene. It has been proven that by simply improving staff behaviours on this topic, patient care improves, and the lives of vulnerable patients could be saved.
Our key learning from the Improvement Academy was that qualitative analysis was important to help the team identify the barriers to implementing the change to hand hygiene practices.
“Fantastic opportunity to access experts in the field to guide you through an improvement project. Great to network and access other specialists who we would not normally be able to liaise with.”
– Julie Dziobon, IPC Clinical Specialist.
Salary saviours
Project aim: Reduce count of monthly late payments and overpayments to NWAS PES and ICC staff pay by 50% by March 2025.
The emotional impact and distress to the staff who experience issues with their pay shouldn’t be underestimated. Added to this are the additional cost to the service in overpayments and late payments.
We have achieved a significant improvement in payroll errors for 111 thanks to the standardisation of their processes and education the team provided to team managers.
“I would recommend the Improvement Academy, as it opens your eyes to looking at situations in different ways and provides motivation to want to make change.”
– Kate Taylor, ESR System Team Leader.
Just 2 more
Project aim: Achieve a 20% reduction in patient conveyance to emergency department by March 2025.
All patients should receive the right care, in the right place, at the right time. We want to eliminate unnecessary hospital handover delays when a patient is suitable for a non-hospital care pathway as an outcome for their treatment.
The team have seen a reduction in see and convey to both emergency department and urgent care services.
“I really feel motivated and enabled to bring positive changes to my area. I love how topics are steered back to our project so we can get improvement knowledge while integrating what we learn.”
– Dan Fry, Senior Paramedic.
Drifters
Project aim: Reduce total time of parent-baby separation due to respiratory distress in full term infants by 50% by April 2025.
Reducing admission rates, length of stay and length of separation between mother and child increases patient welfare and decreases cost pressures.
One notable success story from the project was that the teams’ work enabled a mother and baby to have time together before the child was taken into care. This wouldn’t have been possible before.
“Thank you for providing us with such a wonderful learning and improvement opportunity. This will stay with me to always look for what was once thought to be unachievable – to be able to achieve anything. Thank you for being so supportive. I feel like everyone could benefit from attending the improvement academy. Itis an extremely well-led course that I am so thankful to have been a part of.”
– Danielle Boyd Holt, Neonatal Sister.
Smile…you’re on camera
Project aim: To reduce reported physical assaults against NWAS staff by 50% by September 2025.
Ensuring staff safety will reduce the number of staff off sick due to physical assault, which will increase the number of responding clinicians available to attend to patients.
One key benefit of the project related to incident reporting. We identified a big problem with misreporting in the data. We have made big strides in improving how assaults are recorded to be able to see the real story the data is telling.
“The academy has given me the knowledge and skill to make sustainable and significant change. How to utilise and map data, how to present and how to understand when it’s working, when it isn’t and to not be in fear of failure, but to use this as learning to push us forward.”
– Natalie Samuels, Violence Prevention and Reduction Senior Manager.
Final stop specialists
Project aim: By September 2025, 100% of patients on Ward 11 at Blackpool Victoria will have a documented advanced care plan discussion.
This project is important as advanced care planning allows less aggressive medical care and an improved quality of life for our patients who are near to death.
One key piece of learning for our team was relating to the psychology of change and how best to bring staff and patients along with us in our improvements. We are keen to embed the concept of celebrating success, so that staff feel valued for having appropriate advance care plan discussions.
“I think it’s a really well-structured course. Fab guest speakers – really experienced, inspiring and knowledgeable. I don’t think it can be improved – I’ve really enjoyed it, learnt loads, plenty to take away with me to use in the future and to keep improving services for our patients.”
– Kirsty Jones, Clinical Nurse Specialist – Trinity.
Macclesfield HALO project
The project was set up to attempt to reduce hospital turnaround times and improve hospital arrival screens (HAS) compliance at Macclesfield emergency department. It was led by local senior paramedic team leaders. The challenge faced by NWAS and hospital staff was surrounding the handover of ambulance patients to hospital care. It was felt that by applying improvement science, processes could be made quicker and more efficient.
For the 12 months prior to the start of the project, the average arrival to handover time at Macclesfield emergency department was 36:04 minutes. This was six minutes over the average for the North West region of 30:15minutes and over 22 minutes longer than the “best in class” which was 14:36.
In addition to this, the baseline percentage of HAS compliance for the calendar year prior to starting the project was 17.4%. This made Macclesfield hospital an outlier for this metric, as the best performing hospital had a compliance of 89.8%, and the second worst performing hospital had a compliance of 44.2%.
The tests of change carried out included:
- Engagement with all levels of hospital management from first line emergency department managers up to the board.
- Developing a dialog, collaboration and teamwork to enable us all to work together to find solutions to hospital delays.
- Becoming an advocate for ambulance issues with the hospital, and hospital issues with the ambulance service so that each better understood the other’s difficulties.
- Enabling cohorting, to better release ambulance crews.
- Encouraging the use of the HAS by hospital and NWAS staff.
- Working with ambulance crews to support their decision making, so that more patients were appropriately referred to alternatives to emergency department such as same day emergency care and urgent care services.
The compliance with the ‘handover complete’ process on the HAS screen improved from 17.4% to 87.1 % by 31/05/24. This is an improvement of 69.7%. There was an improvement in the average ambulance arrival to ambulance clear time. This went from an average of 53.4 minutes per patient in 2023, to an average of 46.5 minutes per patient between 01/01/24 and 31/05/24. While this is still 16 minutes over the national standard, it shows an average reduction in time spent by each double crewed ambulance of 6.9 minutes per patient.
Over time, this saving becomes substantial.
- There was also a reduction in the number of patients held in the back of the ambulance waiting to come into the department.
- An increase in the number of patients appropriately referred to non-emergency department alternatives. This reduced the number of patients taken to the emergency department, which helped with patient flow through the department.
East Lancashire care home engagement project
This work is a multi-agency collaborative project which started in October 2023 with care homes across East Lancashire. The aim of the project was to reduce calls to NWAS from care homes and reduce conveyance to the Royal Blackburn hospital by training care home staff to access the appropriate services for residents in their community. This work has included:
- Patient and staff experience and using data to understand where to focus the project.
- Engagement with key stakeholders e.g. care homes, community services, integrated care boards (ICB) etc.
- Education sessions for ten care homes per quarter across Blackburn with Darwen and East Lancashire.
This work has been led by a senior paramedic team leader who has been working with internal and external stakeholders. The project has included training for care homes on the following:
- Introduction to the NWAS call system including, the Ambulance Response Program (ARP) and call categories, service pressures, triage and how can we mitigate harm and keep our patients safe.
- Introduction of clinical frailty score to resident profiles.
- I Stumble App to aid assessment of injured or unwell residents.
- Introduction to wound care, dressings and how to manage onward referral.
- Referral process for the Integrated care Allocation Team and the and 2 Hour Urgent Care Response Service.
- Demonstration of the razor chair and how to access the service.
- Introduction to the referral pathway to the Specialist Medicines Optimisation in Care Homes (SMOCH) Team to discuss how certain medication can contribute to an increased risk of falling, medicines that may be linked with this increased risk and how to refer to the team for review.
- ‘Call before you convey’ and ‘Never say No’ campaign: Familiarisation of the new available pathways and what to expect for care home staff.
- Essential medication and documentation to send with residents to hospital in green bags.
- Champions and Induction packs; how we keep all our staff safe and competent.
In the East Lancashire sector, work has also been undertaken on the ‘Never say No’ campaign to promote referrals into community care and the ‘Call Before you Convey’ project. The patient data for the East Lancashire Sector shows care home attends at Royal Blackburn hospital has significantly reduced and referrals to community services has increased. The ethos of this work is the right care, at the right time, every time.
To summarise, this is the outcome of the projects so far.
- Training delivered to 64 out of 164 care homes.
- Future training is planned to deliver ten care home training sessions per annual quarter across East Lancashire including Blackburn with Darwen.
- A two-hour learning session has been delivered by representatives from each organisation. A learning and information pack has been developed to support care home staff.
- Gold standard induction pack with plans to develop a gold standard care home induction pack.
Closing the loop
As a trust, the North West Ambulance Service (NWAS) is continuously learning and has a wealth of knowledge from investigations and coroners courts, yet there is no reliable assurance that this learning reaches operational staff, and that they embed this learning into their practice. To address this, NWAS has developed a new process to identify and regularly distribute significant patient safety learning to frontline staff, thus closing the loop on learning. Sharing this learning will empower clinicians with critical insights from patient safety incidents, allow for better patient outcomes, build a more knowledgeable workforce and foster a true learning culture.
In October 2023, NWAS implemented the Patient Safety Incident Response Framework (PSIRF), which uses system-based learning in response to patient safety incidents to make improvements and reduce patient harm. A review of current organisational learning showed a reliance on traditional approaches to spreading information, such as bulletins and newsletters. The mobile nature and geographical spread of NWAS’s workforce also means that the methods employed in hospitals to ensure all staff are kept up to date with the latest patient safety information and thinking are not suitable.
The project team needed to establish a bespoke ambulance service model for ensuring that all frontline staff were informed of patient safety learning and alerts. They also needed to create a method of assurance that this learning was becoming embedded in practice. Using Patterson et al.’s (2007) six sources of influence for lasting behavioural change, the project team recognised that the traditional model only uses one form of influence (bulletins and newsletters) to inform staff and ensure changes in their working practice. The new method would combine at least four sources of influence to engage staff. This led to a collaboration between operational, quality improvement and patient safety teams to create the Learning Loop. The team produced regular learning topics, sharing them through various methods, including posters, huddles and social media, utilising as many forms of influence as possible, to effectively engage staff.
The project trial started in January 2024, using improvement methodologies such as the Model for Improvement and Plan, Do, Study, Act cycles. The project aimed to ensure all staff in the trial area received the selected patient safety messages. The project success was measured using dip sample questionnaires. The project also evaluated the effectiveness of the different sources of influence tested. The reported patient safety incidents and level of patient harm were also monitored. In addition, staff were asked for their feedback on the Learning Loop and how it influenced their practice.
Extensive testing and feedback have highlighted how successful the project has been in spreading essential patient safety learning to frontline staff. To evaluate the project’s effectiveness and reach, staff were asked whether they could recall the current Learning Loop topic. Staff awareness of the Learning Loop topic rose from 4% in February 2024 to 50% by November 2024, demonstrating its growing impact in reaching and engaging staff. Qualitative feedback further affirmed the value of the Learning Loop as a ‘conversation starter’ on local and trust wide issues. Staff feedback has also shaped development of the Learning Loop process and informed mechanisms of influence to use in staff engagement.
The right care programme
Background
In May 2024, the trust board approved the refresh of the 22/25 strategy, identifying that in the annual plan there would be an emphasis on urgent and emergency care recovery with ‘Ambulance services are at the heart of the urgency emergency care system’. ‘Right Care’ is central to system-wide approach to transformation arising from national drivers and local UEC recovery initiatives.
The Right Care Programme (formally Reducing Avoidable Conveyance Programme) was established with several priority workstreams to seek to address this. There are nine dedicated workstreams that allow the trust to respond to the need to reduce pressure on emergency departments, support our staff both clinically and psychologically, optimise the way in which we respond to management of healthcare professional activity, and enhance our digital capability as we interact with other providers.
Challenges and benefits
The overall aim of the programme is to provide the ‘right care’ to our patients. Whilst there will always be a need to convey our most unwell patients to hospital, our focus must continue to ensure we are able to manage our patients using alternative pathways of care, and in the community whenever possible.
This programme seeks to aide our clinicians in making clinically appropriate assessments and providing routes into the most appropriate alternative pathways of care. There are numerous benefits to both the patient, NWAS, our partners and the wider health care system in achieving this aim. Not least the patient receiving the care commensurate to their need, moreover multiple benefits to the wider health care system including a reduction in handover delays at emergency departments and less on scene time for crews resulting in a positive impact on our ability to meet response times for time critical patients. The programme also aims to reduce variation across the trust footprint where appropriate considering the differing needs of patient population across the regions we serve. These in themselves have a degree of variation due to demographics, deprivation and geographical challenges. As such, a one size fits all approach is not suitable.
Results
The Right Care team has graduated from the trust’s inaugural Quality Improvement Academy, working with the West Cheshire sector to manage elderly patients in their homes whenever possible. Close collaborative working with the emergency care improvement team and local urgent care response teams has allowed the trust to manage over 75% of patients without attending an emergency department. We are now working to upscale these initiatives, taking valuable learning into our partnerships across the North West.
Quality aims 25/26
The priority areas for improvement during 25/26 aligned with the Quality Strategy include:
Safety first
- Focus on delivering national and local priorities in line with the Patient Safety Incident Response Framework (PSIRF).
What success looks like:
Teams will be clear on how the PSIRF framework will support learning and improvement from patient safety events nationally whilst focusing on the local priorities of:
- Managing a cardiac arrest.
- Clinical assessment and treatment of women during maternity care that is managed outside of JRCALC guideline of trust policy.
- Harm resulting from a patient refusal where there is an absence of documented informed consent/refusal/mental capacity assessment.
Highly effective care
- Continue to strengthen our delivery against the Care Quality Commission (CQC) assessment framework for safety, effectiveness, patient centeredness, responsiveness and well-led in readiness for future inspection.
- Improve the processes associated with medicines management including controlled drugs.
What success looks like:
- Our leaders will be prepared with an understanding of the Single Assessment Framework (the new framework for assessment for all healthcare organisations). This process will provide a focus to empower staff to build on their successes and identify areas for improvement to ensure the quality of care we deliver is safe, effective, patient centred and responsive. We will also build our evidence of compliance against each of the new ‘we’ statements.
- The risks associated with medicines management and controlled drugs will be mitigated with the procurement of a digital stock management system and the submission of a business case to procure an electronic controlled drugs register.
Improving safety culture for staff and patients
- Continue building capacity and application of improvement methodology from board to frontline to strengthen delivery of strategic objectives.
What success looks like:
- We will build on the success of the improvement academy by training more teams on the science of improvement methodology using real time improvement projects to embed theory into practice.
- We will deliver improvement training to the wider workforce and ensure this is recorded in the Electronic Staff Record (ESR), to include the number of staff trained in improvement science. This will ensure all staff have the knowledge and skills to be able to identify area for improvement and implement change through a proven model of improvement methodology.
Formal statements on quality
Review of services
During 24/25 we have provided and/or sub-contracted NHS urgent and emergency care services across the North West. The income generated by the NHS services reviewed represents 100% of the total income generated from the provision of relevant health services by our trust for this period. We have reviewed all the data available on the quality of care in the NHS services provided.
Participation in clinical audits
This year has seen the Clinical Audit team moved to the Medical directorate. This enables a reshaping of the team with the introduction of a senior clinical audit manager, which is intended to link to clinical leaders across the organisation to better integrate performance and results in clinical outcomes to local leadership teams. As such we hope to see greater collaborative working in the future to further enhance clinical outcome data and performance. Furthermore, a project has been initiated to replace the current clinical audit tool, and we are scoping any improvements or efficiencies that this may bring in the future.
The clinical leadership and specialist clinical teams work alongside the clinical audit team to produce a yearly local clinical audit workplan. There has been participation from teams such as public health, maternity, digital, patient safety and critical care to enable a wide variety of local audits to be completed and subsequently driving improvements in clinical care.
Following a local audit completed around management of asthma in 23/24 education was provided to operational staff to improve compliance. The reaudit completed this year showed improvement across all metrics measured from 19.1% receiving excellent care in 23/24 to 52.6% receiving excellent care in 24/25. Furthermore, audits relating to thermoregulation of newborns has help contribute towards measuring the impact of this year’s mandatory training cycle and support a case for change around the equipment available to frontline clinicians. The continued monitoring of that audit will allow for the impact of the change to be measured effectively.
Additionally, 24/25 saw the working relationship between the Clinical Audit team and North West Air Ambulance (NWAA) increased through attendance at the NWAA Research and Audit group, supporting NWAA to explore the registration of additional audits on top of their ongoing audit portfolio.
Participation in clinical research
North West Ambulance Service develops, hosts, and delivers research that has a focus on pre-hospital urgent and emergency healthcare, injuries, and other clinical specialities. We also explore non-clinical research opportunities involving the organisation and our workforce. From clinical trials looking at drug administration routes in patients with out-of-hospital cardiac arrest, to research studies exploring staff views on clinical decision-making when attending older adults who have fallen, NWAS actively contributes to the development of the evidence-base that helps improve the care and experience of all our patients.
The executive medical director is the executive lead for research. Under the leadership of the research lead, consultant paramedic (Medical directorate), the Research and Development (R&D) team ensures that research and service evaluation projects are developed, set-up and conducted in line with national NHS research regulation/standards, and local policy/procedures. This is achieved with the expert input and support of colleagues from directorates and departments across the organisation.
The R&D team has continued to make strides in embedding research across the organisation. Income was secured from the National Institute for Health and Care Research (NIHR) for the new substantive position of senior research fellow and two research paramedics who promote and deliver studies across the organisation, ensuring that patients, staff, and the public can take part in research. For the fifth consecutive year, the trust successfully triggered NIHR Research Capability Funding (RCF) by successfully recruiting participants to NIHR Research Delivery Network (RDN) Portfolio research studies beyond the expected threshold. The purpose of NIHR RCF is to help research-active NHS organisations to act flexibly and strategically to maintain research capacity and capability.
We strengthened our partnership with NIHR RDN North West, the new entity formed from the merger of former NIHR Clinical Research Networks Greater Manchester and North West Coast. We continued to work with our local NIHR Applied Research Collaborations, health and care providers, higher education institutions and other external stakeholders to cultivate research collaborations. We remained an active member of the Association of Ambulance Chief Executives (AACE), National Ambulance Research Steering Group (NARSG), a collaboration between all UK ambulance services that provides a forum to foster research partnerships. As a result of stakeholder engagement, NWAS colleagues were listed as co- applicants for successful NIHR bids, and new bids in development, creating a pipeline for future research opportunities for our organisation.
The R&D team continuously seek opportunities to engage with patients, staff, the public, and research communities both locally and nationally to ensure that NWAS is visible as a research active organisation. The R&D team represented NWAS at internal and external events to raise awareness of research taking place across the trust. We publicised research opportunities, successes, and achievements both internally and externally through various communications channels including trust news bulletins, websites, social media and the NWAS staff app.
Performance in clinical research
In 24/25, we opened 11 new research studies that were approved by the NHS Health Research Authority (HRA). Two of the newly approved research studies were NIHR RDN Portfolio studies.
NWAS had a total of five NIHR RDN Portfolio studies open to recruitment in the financial year 24/25 to which we successfully recruited 1,067 research participants including staff, patients and the public.
In 24/25 we achieved our highest ever participant recruitment to NIHR RDN Portfolio studies in the trust’s history. This was a result of the R&D team building capacity in its infrastructure, creating dedicated roles that enable the trust to engage with potential new research partners and identify opportunities for research collaboration, but also research paramedic resource that allows for research to be championed and promoted across the organisation.
| National Institute for Health Research Research Delivery Network Portfolio Performance 23/24 | ||||
| Financial Year | 21/22 | 22/23 | 23/24 | 24/25 |
| Number of Studies Open to Recruitment | 9 | 10 | 9 | 5 |
| Number of Participants | 630 | 923 | 936 | 1067 |
The two new NIHR RDN Portfolio research studies we confirmed our capacity and capability to deliver in the 24/25 included:
- AMBOFALL: Ambulance response to older adults who have fallen – a mixed-methods study.
- Jay’s study: Developing tailored implementation of a personalised safety planning toolkit for adults experiencing self-harm and suicidality.
In 24/25, confirmation of capacity and capability was issued for nine non-portfolio studies:
- HOTZONE: Improving patient outcome in the ‘hot zone’ during a major incident – a mixed methods medical research approach.
- The Bump Study: Children’s traumatic brain injury management and triage in the prehospital setting – a qualitative study.
- Complex PTSD and Psychotic-Like Experiences in UK Paramedics.
- Moral Injury Pilot Survey: Understanding the causes, processes, and consequences in the UK ambulance service.
- A mixed methods exploration of prehospital research culture and capacity building in UK NHS ambulance services.
- Frontline ambulance service staff cultural competence.
- Enhancing prehospital recognition of intracerebral haemorrhage and stroke mimics.
- Use and opinions’ concerning medicines related errors, monitoring and audit tools used to assess medicines optimisation within care homes in England.
- The mental health and wellbeing of NHS call-handlers and dispatchers (CHDs) working in the emergency (999) and urgent (111) helplines in England.
CQC rating
We welcomed the CQC whilst they carried out a focussed inspection of Lancashire and South Cumbria Integrated Care System (ICS) and Cheshire and Merseyside ICS in 2022. The service lines included: emergency and urgent care, emergency operations centre and NHS 111. Whilst this was not a well led inspection, we have maintained our ‘Good’ rating.
| Safe | Effective | Caring | Responsive | Well-led | Overall | |
| Provider Wide | Good | Good | Good | Good | Good | Good |
| Emergency and Urgent Care | Good June 2020 | Good June 2020 | Good June 2020 | Outstanding June 2020 | Good June 2020 | Good June 2020 |
| Emergency Operations Centre | Good June 2020 | Good June 2020 | Good June 2020 | Good June 2020 | Good June 2020 | Good June 2020 |
| Patient Transport Service | Good Jan 2017 | Good Jan 2017 | N/A | Good Jan 2017 | Requires improvement Jan 2017 | Good Jan 2017 |
| Resilience | Good Nov 2018 | Good Nov 2018 | Good | Good Nov 2018 | Good Nov 2018 | Good Nov 2018 |
| 111 | Good Jan 2017 | Good Jan 2017 | Good Jan 2017 | Good Jan 2017 | Good Jan 2017 | Good Jan 2017 |
In 2023, the Care Quality Commission (CQC) redesigned their assessment process and introduced a new system called the Single Assessment Framework (SAF). The CQC began to implement the SAF in the third quarter of 2023, however, full deployment was delayed following feedback and restructuring within the CQC.
During 24/25, North West Ambulance Service has continued regular, routine engagement meetings and enquiries with the CQC.
NWAS has actively worked on adapting and developing our own internal assurance processes in response to the CQC’s changes, ensuring evidence categories are measured, as set out by the CQC Quality Statements. NWAS will adapt as required, to ensure that as the CQC’s approach evolves, our own assurance processes evolve in parallel.
System Oversight Framework (SOF)
NHS England’s System Oversight Framework provides the framework for overseeing systems and providers and identifies potential support needs. The framework is built around five national themes that reflect the ambitions of the NHS Long Term Plan, NHS People Plan and the shared local ambitions and priorities of individual ICSs:
- Quality of care, access and outcomes.
- Preventing ill health and reducing inequalities.
- Finance and use of resources.
- People.
- Leadership and capability.
As part of NHS England’s oversight, performance is monitored across each of these themes whereby providers are allocated to one of four segments that identify the nature of support needs. Segment one reflects no specific needs and segment four reflects providers that require mandated intensive support.
NHS England has assessed that we are segment two, which by default, all ICSs and trusts are allocated unless the criteria for moving into another segment are met.
Further information in relation to the Oversight Framework is on the NHS website.
Stakeholder feedback
We work in collaboration with all partners and the Quality Account has been shared with our external provider organisations including commissioners, councils, Patient and Public Panel members, Overview and Scrutiny Committee, Healthwatch and neighbouring ambulance services.
Statement from the Lancashire and South Cumbria Integrated Care Board
Introduction
“Lancashire and South Cumbria Integrated Care Board (ICB) hosts the Ambulance and NHS 111 Commissioning Team (ACT) who work on behalf of the ICBs that make up the North West (NW) region. In doing this it ensures that robust commissioning, quality, contract and performance management is in place to enable and support North West Ambulance Service (NWAS) to provide effective services to the residents of the North West.
These services comprise:
- Paramedic Emergency Service (PES): the 999 ambulance service
- NHS 111 services
- Patient Transport Services (PTS): enabling eligible patients to access outpatient, discharge and other hospital appointments for Greater Manchester, Merseyside, Lancashire and Cumbria. Services for Cheshire are not provided by NWAS.
The ACT welcomes the opportunity to review and support the 2024/25 NWAS Quality Account.
Ambulance and NHS 111 Services Governance
NWAS provides services across five “county” areas; Cumbria, Lancashire, Cheshire, Merseyside and Greater Manchester. This is a complex geography which contains 3 full ICB footprints (Lancashire and South Cumbria, Greater Manchester, Cheshire and Merseyside), and 2 partial footprints (North Cumbria, which forms part of North East and North Cumbria ICB, and Glossop which forms part of Derby and Derbyshire ICB). NWAS supports a diverse NW population of circa 7.5 million with many rural and isolated areas with lower population levels and inner city areas like Manchester and Liverpool which have densely populated areas. With over 50 languages spoken in the region and such a diverse population the ICB acknowledges NWAS’ commitment and emphasis on supporting equality and diversity for its population.
The Strategic Partnership Transformation Board (SPTB) operates on behalf of the 5 ICBs and is attended by a designated ICB lead at executive level. The primary function of SPTB is to assure commissioners that NWAS are meeting all required national targets and KPIs and delivering safe and effective services. The Regional Ambulance and 111 Quality Group (RAQG) and Finance, Performance and Contracting Group, which are sub-committees of SPTB and report to it, gain this assurance from NWAS and ensure the ICBs remain sighted on the quality of care and performance levels NWAS have provided.
2024/25 Quality Account Overview
Commissioners wish to acknowledge that the NWAS 2024/25 Quality Account is a comprehensive, well-presented and easy to read account.
It has been another challenging year, not only for NWAS but for the whole of the NHS, especially Urgent and Emergency Care (UEC), with winter pressures again causing challenges to deliver timely care to patients. Despite this NWAS has been one of the few English ambulance services that has achieved the UEC Recovery Plan (B2034-delivery-plan-for-recovering-urgent-and-emergency-care-services.pdf) target of 30 minutes for emergency (999) Category 2 response times. This has taken a lot of hard work, not only from NWAS and all of their staff and volunteers, but also through collaborative work undertaken with ICBs, acute trusts, and other external stakeholders. Work to reduce hospital handover times where possible and safely find the most appropriate care for their patients calling 999 or 111 aligns to NWAS’ vision of ‘Right Care, Right Time in the Right Place.’
The ICB acknowledges the hard work undertaken by NWAS to maintain its Care Quality Commission (CQC) rating of ‘Good’ and its commitment to strive to achieve ‘Outstanding’ within 3 years. NWAS’ core values of ‘working together’, ‘being our best’ and ‘making a difference’ alongside their improvement work and digital innovation, will aid the achievement of this goal.
Quality Strategy
The ICB welcomes NWAS’ commitment, as part of their Quality Strategy, to embed strong leadership and ensure that their quality ambitions are fully realised, including the appointment of a new Chief Executive with many years’ personal experience of NWAS. The Quality Account lays out NWAS’ aims for 2024/25, which were:
- Safer Care
- Highly Effective Care
- Patient Centred Care
- Quality Standards and Compliance
- Continuous Improvement
- Equality, Diversity and Inclusion
It was pleasing to read how NWAS have achieved these within the Quality Account, including their extensive engagement with staff and stakeholders, as well as the steps taken to understand patients’ experiences. This is reflected in the high number of Friends and Family Test responses received with really positive results across all service lines, and the introduction of Patient Safety Partners. The introduction of Safety Culture surveys to drive improvement, the development of a new Clinical Supervision Framework to support staff to deliver highly effective care, and the launching of the Improvement Academy are just a small sample of this work and are well received by commissioners.
Operational Performance
Commissioners acknowledge the ongoing work by NWAS to integrate their contact centres across all service lines, to ensure equity to patients, no matter how they access NWAS’ services. This integration not only better supports patients’ needs but at this time of NHS reconfiguration, service reviews and financial challenges, integration should ensure improvement in productivity and operational efficiency.
Continuing on the theme of integration of service lines, Commissioners welcome the introduction of digital improvements that flag to the Patient Transport Service if a patient booked for transport has contacted other NWAS service lines via 999 or 111 and therefore may not now require transport, for example if they have been admitted to hospital. Another example of increasing operational efficiency and freeing up availability of vehicles for other patients or reducing waiting times for existing ones.
NHS 111
The Quality Account outlines the improved position of NHS 111 call handling, with 83% of calls in 2024/25 answered within 60 seconds, a 33% improvement on the previous year. There has also been a 10% reduction in the call abandonment rate (when a caller disconnects before the call is answered) to an all-time low of 2.7%. These are real indicators that calls are being answered in a timely manner and can only deliver better patient experience. Commissioners acknowledge the work undertaken within 111 to significantly improve sickness and staff attrition levels, and to support their staff to help achieve these strong performance levels. Although not included in the Quality Account this work has been acknowledged nationally with NWAS presenting on their work to the Ambulance Culture Review Board.
Paramedic Emergency Service (PES 999)
999 call demand continues to fall in 2024/25, although there is seasonal variation. Commissioners also acknowledge that where more timely ambulance responses occur that there are fewer repeat calls. Call pick up times in 999 calls are strong, with NWAS achieving 97.8% of 999 calls answered in under 5 seconds, ensuring those calling for the most life threatening situations, such as cardiac arrest, can be given lifesaving advice sooner and receive a more timely allocation of emergency responders, as well as delivering good patient experience. Commissioners appreciate the work this has taken to achieve and has resulted in NWAS continually being ranked one of the best performing ambulance services in England for this measure.
There has only been slight variation in the number of 999 incidents over the past few years with a small drop of 0.3% on the previous year, meaning NWAS dealt with 1,118,433 emergency incidents in 2024/25, making it one of the busiest emergency ambulance services in England.
The Quality Account outlines how NWAS supported 15% of 999 incidents over the telephone, either by giving advice or signposting patients to appropriate local services. This in turn reduces the number of ambulances that need to be dispatched meaning that emergency ambulances are more readily available for those with life threatening presentations who need time critical interventions. It also assists in achieving the national Ambulance Response Programme (ARP) standards. NWAS have seen an improvement in response times on last year for Category 1, 3 and 4 calls. Although there has been an increase in response times for Category 2 calls (which includes potential strokes and heart attacks) as outlined earlier NWAS have achieved the UEC Recovery Plan goal of a 30 minute mean Category 2 response time for 2024/25.
The UEC Recovery Plan also acknowledges the impact of delayed hospital handover of ambulance patients impacts negatively on ambulance availability and in turn the ability for ambulance services to respond to waiting emergencies in the community. Commissioners acknowledge the collaborative work undertaken in the past 12 months with NWAS, ICBs and hospital providers to improve these times, however there is wide variation in the improvement seen, impacting on NWAS. Commissioners will support further improvements in 2025/26 with the continuation of the ICB-lead Ambulance Improvement Groups.
Although performance has improved, and NWAS should be congratulated on their continued drive for improvement, it is noted that there is still a way to go to achieve the response standards envisaged in ARP. Commissioners, via SPTB, will continue to support NWAS to achieve this via delivery of their main priorities to increase the number of patients supported safely and appropriately closer to home rather than being transported to hospital, developing a single point of access to identify the most appropriate service to support patient needs, and reducing the variation in hospital handover times through achieving the national hospital handover standard and eliminating patients waiting in ambulances to access A&E.
Patient Transport Services (PTS)
NWAS holds the PTS contract for Greater Manchester, Merseyside, Lancashire and Cumbria. Due to ongoing re-procurement across the region these have been extended until 31st March 2026.
In last year’s ICB statement we highlighted NWAS’ reliance on private ambulance providers following some of the impacts COVID still had on PTS, and the NWAS commitment to reduce this. It is pleasing to see in this year’s Quality Account that the use of private providers has fallen by 50%. It was also encouraging to see the introduction of digital improvements with the utilisation of automated SMS text messaging to remind patients of their booked PTS journey and confirm if it still needed, so reducing the number of journeys where ambulances are dispatched unnecessarily.
Last year’s Quality Account outlined the aim for PTS to return to pre-COVID levels, and there has been improvement in activity levels. However, Commissioners acknowledge that some of this activity has changed with some longer journey times for patients needing to trave further for their appointments.
Patient Experience
It was really encouraging to see that NWAS received 1289 compliments from patients in 2024/25, with 979 involving clinical treatment. As outlined earlier it is also good to see such a high number of Friends and Family test returns for all service lines, with a total of 22,394 received, of which over 90% felt they were treated with dignity, respect and compassion.
Commissioners note the Patient and Public Panel (PPP) inclusion and its high level of members across the NW alongside NWAS’ acknowledgement that this feedback and lived experience is invaluable to them. NWAS have plans to further development this in 2024/25 and widen the membership diversity.
Commissioners also welcome NWAS’ patient and public engagement, gaining qualitative feedback that is used to drive further improvement as well as educating local communities with cardio-pulmonary resuscitation (CPR) training, winter health messaging and self-care advice.
Summary
It has been another challenging 12 months for the NHS as a system, the North West, and for NWAS. However, there are continuing signs of improvements for NWAS with improved achievement of national standards.
The next 12 months will continue to see changes within the NHS with Working Together in 2025/26 to lay Foundations for Reform, changes and re-structuring NHS England, the ICBs, and with providers and the publication of the 10 year Health Plan. However, as can be seen from their Quality Account, NWAS are in a strong position to deliver the requirements for national standards and support the population of the North West, whilst delivering excellent quality of care when their help is needed.
Commissioners would like to thank NWAS and all their staff for the hard work undertaken during 2024/25 and the support they have given to the population of the North West, outlined well in this Quality Account.”
Statement from Lancashire County Council Democratic Services
“Many thanks for early sight of the NWAS quality account report. As you will be aware, the county council is currently coming towards the end of the election process, with the outcome due on Friday.
As a result, the Health and Adult Services Scrutiny Committee would be unable to comment on this years Quality Account. However, the committee will remain engaged and keen to maintain ongoing dialogue throughout 2025/26.”
Statement from North West Ambulance Service Patient, Public Panel members
“What a comprehensive account, I am blown away. I thought everything was explanatory and whilst I know that this is not the final draft, whoever carried it out has done an amazing job collating the information together and then actually bringing it all together.”
“I find the report clear, concise & easy to navigate. The information is presented in a logical sequence. I was surprised to see however that 999 calls are seeing a decrease year on year, but this could be due to the increasing efficiencies of the 111 service! Good to see also that the calls are picked up within one second, very impressive.”
Statement from three local Healthwatch Westmorland and Furness, Cumberland, and Lancashire
“I was pleased to read about the work done by the Patient Engagement Team, particularly that there is a commitment to using face-to-face methods to compliment digital. I hope that, despite low completion rates for physical postcards, that these will continue to be provided for those who are ‘digitally excluded’, and that new, accessible sites for placement, support for completion, and collection will be considered.
It’s heartening that patient satisfaction with treatment (dignity, compassion and respect), as well as overall satisfaction and experience are so high, and have either stayed the same or risen since quarter one. From the personal stories shared it is also clear that reasonable adjustments are made by paramedics and other staff, these efforts are appreciated, and that there is a high regard for the ambulance service generally.
Healthwatch Westmorland and Furness supported NWAS with a patient experience survey on Alston Moor from May 2023 to April 2024 about the pilot response model there, and these findings are in line with those.
I noted the comment on the need to get more feedback from different demographics, including young people and those with learning disabilities. It’s good to read about the innovative ways of gathering patient stories, such as video.
Regarding PALS, I hope that the response to complaints will continue to evolve, including making reasonable adjustments for communication to meet the Accessible Information Standard, and that the availability of Language Line, BSL and Easy Read materials are promoted on-site and through different media.
Generally, it is also good to read that challenges facing Trust teams, such as those around call response times are being met, and that a handover improvement scheme is in place to address this patient safety issue.”
Appendices
Glossary of terms
AACE. The Association of Ambulance Chief Executives provides ambulance services with a central organisation that supports, coordinates and implements nationally agreed policy.
Advanced Paramedics (APs). Advanced paramedics offer a high level of clinical skills and leadership. They co-ordinate and provide clinical advice for some of the more complex incidents we attend, whilst also being responsible for a team of senior paramedics.
ARP. Ambulance Response Programme: In 2017, following the largest clinical ambulance trials in the world, NHS England implemented new ambulance standards across the country. This was to ensure the sickest patients get the fastest response and that all patients get the right response first time.
ALO. Ambulance liaison officer acts as a bridge between the ambulance service and ambulance teams.
AQI. Ambulance Quality Indicators are quality measures used to access the quality of ambulance services focusing on the speed of response and quality of care provided.
BAME. Black, asian and minority ethnic is a term used in the UK to describe non white ethnic groups
BAF. Board assurance framework is used to record and report an organisational key strategic objectives, risks, controls and assurances to the board.
C1. Category one: An immediate response to a life-threatening condition, such as cardiac or respiratory arrest. Response time to 90% of all incidents is 15 minutes.
C2. Category two: A serious condition, such as stroke or chest pain, which may require rapid assessment and/or urgent transport. Response time to 90% of all incidents is 40 minutes.
C3. Category three: An urgent problem, such as an uncomplicated diabetic issue, which requires treatment and transport to an acute setting. Response time to 90% of all incidents is two hours.
C4. Category four: A non-urgent problem, such as stable clinical cases, which requires transportation to a hospital ward or clinic. Response time to 90% of all incidents is three hours.
Cardiac arrest. A medical condition wherein the heart stops beating effectively, requiring CPR and sometimes requiring defibrillation.
CCA. Civil Contingencies Act, 2004 requires NHS organisations and providers of NHS-funded care, to show that they can deal with a wide range of incidents and emergencies that could affect health or patient care while maintaining services.
CEO. Chief executive officer.
Cleric. Ambulance software solution.
CFR. Community first responder. A member of the public who volunteers to provide an immediate response and first aid to patients requesting ambulance assistance.
CHUB. The clinical hub is a department within our emergency operations centres that is a multidisciplinary team including clinicians, dispatchers, navigators and managers.
CIH. Complex incident hub.
Cohorting. A process where one ambulance crew looks after a few patients to free up other crews
Community first responder (CFR). A member of the public who volunteers to provide an immediate response and first aid to patients requesting ambulance assistance.
CPR. Cardiopulmonary resuscitation is a lifesaving technique used when someone’s breathing or heart has stopped.
CQC. Care Quality Commission is the independent regulator of all health and social care services in England.
CSTF. NHS core skills training framework which sets out NHS England training approach to statutory and mandatory educational topics.
DCIQ. Datix Cloud IQ is a profound shift in focus for a healthcare risk management application, moving beyond the simple capture and review of data on adverse outcomes towards a managed process of exposing and resolving the issues that lead to those outcomes.
Directory of Services (DoS). A central directory that is integrated with NHS Pathways and is automatically accessed if the patient does not require an ambulance or by any attending clinician in the urgent and emergency care services.
DSPT. The Data Security and Protection Toolkit is an online self-assessment tool that allows organisations to measure their performance against the National Data Guardian’s 10 data security standards. All organisations that have access to NHS patient data and systems must use this toolkit to provide assurance that they are practising good data security, and that personal information is handled correctly.
Duty of candour. Every health and care professional must be open and honest with patients and people in their care when something that goes wrong with their treatment or care causes, or has the potential to cause, harm or distress.
ECG. Electrocardiogram (ECG) is a simple test used to check a heart’s rhythm and electrical activity.
ED. The emergency department is for serious injuries and life-threatening emergencies.
EMT. The purpose of the emergency medical technician role is to assist in the delivery of high-quality and effective pre-hospital clinical care, responding to 999 emergencies, inter-hospital transfers and urgent hospital admissions.
EOC. Emergency operational control receives and responds to 999 calls and other calls for ambulance service assistance.
EPR. Electronic patient record is a periodic health care record of a single individual, provided mainly by one healthcare organisation.
EPS. Enhanced priority service is a service for PTS patients receiving renal dialysis or cancer treatment.
ESR. Electronic staff record is a payroll database system commissioned by the Department of Health and Social Care that NHS organisations are entitled to use.
FAST. A simple test for the presence of a stroke – face, arms, speech, time.
FFT. The NHS Friends and Family Test is to help service providers and commissioners understand whether patients are happy with the service provided, or where improvements are needed. It is a quick and anonymous way to give your views after receiving NHS care or treatment.
Fit testing. Face fit testing is required for employees wearing tight-fighting respirators to ensure individual fit and good seal between face and respirator.
FTSU. Freedom to Speak Up (FTSU) is about encouraging a positive culture where people feel they can speak up and their voices will be heard, and their suggestions acted upon. Speaking up is about anything that gets in the way of providing good care.
HALO module. Hospital arrival screens (HAS) are used to show what time an ambulance arrives at hospital; what time a patient handover occurs and what time a vehicle is cleared to attend another job. Since October 2022, hospital arrival screens have a new capability to capture when patient delays occur via the HALO module.
Hear and treat. An incident when a person does not require an ambulance, but a clinician is able to provide treatment and advice over the phone.
HSE. Health and Safety Executive is a regulatory body to ensure safe working practices are adhered to.
HSJ. Health Service Journal is a news service that covers policy and management in the NHS.
ICB. Each Integrated care system (ICS) will have an Integrated Care Board (ICB), a statutory organisation bringing the NHS together locally to improve population health and establish shared strategic priorities within the NHS.
ICC. Integrated contact centres. Our 111, 999, patient transport service (PTS) and clinical hub call-handling services have been brought together as one integrated contact centre.
ICS. Integrated care systems are partnerships between the organisations that meet health and care needs across an area, to coordinate services and to plan in a way that improves population health and reduces inequalities between different groups.
IPC. Infection prevention and control.
JRCALC. Joint Royal Colleges Ambulance Liaison Committees’ role is to provide robust clinical speciality advice to ambulance services within the UK and it publishes regularly updated clinical guidelines.
LADO. A local authority designated official who is responsible for overseeing the management of allegations and concerns about professional or volunteers who work with children
LD&A. Learning Disability & Autism.
LeDeR. Learning from Life and Death Reviews. This is a national service improvement program in England that’s reviews the deaths of people with learning disabilities and autism people so that services can be improved.
LfD. Learning from deaths process sets out the practices used within our service to review and learn from the deaths of patients who had been under our care. The Clinical Audit team and senior clinicians lead the process. This learning ensures we can protect future patients from avoidable harm, reduce unwarranted variation and provide truly patient-centred care.
MBRRACE-UK. Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries collaboration. MBRRACE-UK is the collaboration appointed by the Healthcare Quality Improvement Partnership (HQIP) to run the national Maternal, Newborn and Infant clinical Outcome Review Programme (MNI-CORP) which continues the national programme of work conducting surveillance and investigating the causes of maternal deaths, stillbirths and infant deaths.
MHRV. Mental health response vehicles are a new, first-line response service to attend patients presenting via 999 or 111 using a new national specification of mental health vehicle, to patients who are requiring an ambulance response, where the primary complaint is a mental health concern.
NACQI/ACQI/AQI. National Ambulance Clinical Quality Indicator.
NARSG. National Ambulance Research Steering Group. A collaboration between all UK ambulance services that provides a forum to foster research partnerships
NEWS. National Early Warning Score is a tool developed by the Royal College of Physicians which improves the detection and response to clinical deterioration in adult patients and is a key element of patient safety and improving patient outcomes.
MEWS. Modified Early Warning Score is a tool which improves the detection and response to clinical deterioration in pregnant or newly delivered women
NHS England. NHS England leads the National Health Service (NHS) in England.
NHS Pathways. NHS Pathways is a clinical tool used for assessing, triaging and directing the public to urgent and emergency care services.
NIHR Applied Research Collaborations. The National Institute for Health Research (NIHR) is the nation’s largest funder of health and care research and provides the people, facilities and technology that enables research to thrive. NIHR Applied Research Collaborations (ARCs) support applied health and care research that responds to and meets, the needs of local populations and local health and care systems.
NIHR CRN. National Institute for Health Research Clinical Research Network (CRN) supports patients, the public and health and care organisations across England to participate in high-quality research, thereby advancing knowledge and improving care. The CRN is comprised of 15 local clinical research networks and 30 specialties who coordinate and support the delivery of high-quality research both by geography and therapy area. National leadership and coordination are provided through the CRN Coordinating Centre.
NWAS. North West Ambulance Service NHS Trust.
PSIRF. The Patient Safety Incident Response Framework outlines how providers should respond to patient safety incidents and how and when a patient safety investigation should be conducted.
PSII. Patient Safety Investigation is a structured process used in healthcare to examine a specific patient incident.
Paramedic. A state registered ambulance healthcare professional.
PDSA cycles. The Plan-Do-Study-Act cycle is shorthand for testing a change i.e., by planning it, trying it, observing the results and acting on what is learned. This is the scientific method, used for action-oriented learning.
PGD. Patient Group Directions provide a legal framework that allows some registered health professionals to supply and/or administer specified medicines to a pre-defined group of patients, without them having to see a prescriber.
PES. Paramedic emergency service responds to 999 emergency ambulance calls.
PHSO. Parliamentary Service Ombudsman independently investigate complaints about UK government departments, other public organisations and the NHS in England.
Power BI. Power BI is a collection of software services, apps and connectors that work together to turn your unrelated sources of data into coherent, visually immersive and interactive insights.
PPP. Our Patient and Public Panel consists of volunteers who live in the North West of England and are involved in public and patient engagement activities e.g. responding to surveys, giving feedback on publications, focus groups activities, attending committees or formal meetings.
PRISM. Pan Regional Information Sharing Mechanism.
PTS. Patient transport service is a non-emergency transport service that provides for hospital transfers, discharges and outpatients appointments for those patients unable to make their own travel arrangements.
QI. The term ‘quality improvement’ refers to the systematic use of methods and tools to try to continuously improve quality of care and outcomes for patients. There are a range of different methods and tools, such as Lean, Six Sigma and the Institute for Healthcare Improvement’s Model for Improvement.
RCF. Research capability funding.
RIDDOR. Reporting of injuries, diseases and dangerous occurrences regulations
ROSC. Return of spontaneous circulation.
RPE. Respiratory protective equipment
SafeCheck. Is an electronic database which was originally designed to replace paper process checks e.g. vehicle, equipment and medicine check book. SafeCheck is now used to capture routine audit work e.g., infection prevention and control.
See and convey ED. Any patient conveyed to a consultant-led emergency department (or if department is not specified) including stroke/PPCI units.
See and convey non-ED. Any incident with any patient conveyed to any facility other than an emergency depatment, including urgent treatment centres, minor injuries units, walk in centres, emergency, medical, or surgical assessment units, same day emergency care, hospital to hospice.
See and treat. An incident with face-to-face response, but no patient conveyed including patient refusal, deceased, or not found, ambulance staff arranged an alternative appointment or follow up visit, or ambulance staff attended and gave clinical advice.
SMDR. Service model delivery review
Single Assessment Framework. The Care Quality Commission (CQC) has introduced a new way of assessing health and social care services in England, known as the Single Assessment Framework (SAF).
SJR. Structured judgement reviews are a methodology used for investigations.
SMART programme. Our internal digital and quality improvement programme.
SPTLs. Senior paramedic team leader working as part of a crew or as a solo responder to attend urgent and critical emergency situations in a variety of environments. They use advanced clinical skills and manage a clinical team.
Statistical process control. An analytical technique that plots data over time. It helps us understand variation and in so doing guides us to take the most appropriate action.
STEMI. ST segment elevation myocardial infarction is a life-threatening heart attack.
Stroke. Blockage or bleeding of the blood vessels in the brain that can lead to death or disability.
UEC. Urgent and emergency care (UEC) services perform a critical role in keeping the population healthy.
Urgent care service. Part of the paramedic emergency service which provides responses to lower acuity calls.
Utstein. Cardiac arrest and CPR outcome reporting process.
Research publications 24/25
The following research publications were either authored or co-authored by staff at North West Ambulance Service NHS Trustin the financial year 24/25:
Alqurashi, N., Bell, S., Alzahrani, A., Lecky, F., Wibberley, C., & Body, R. (2025). Current challenges and future opportunities in on-scene prehospital triage of traumatic brain injury patients: A qualitative study in the UK. Injury [online], 112203. Available at: https://doi.org/10.1016/j.injury.2025.112203
Alqurashi, N., Bell, S., Carley, S. D., Lecky, F., & Body, R. (2024). Head Injury Evaluation and Ambulance Diagnosis (HOME) Study protocol: a feasibility study assessing the implementation of the Canadian CT Head Rule in the prehospital setting. BMJ open [online], 14(6), e077191. Available at: https://doi.org/10.1136/bmjopen-2023-077191
Barrett, J. W., Eastley, K. B., Herbland, A., Owen, P., Naeem, S., Mortimer, C., King, J., Foster, T., Rees, N., Rosser, A., Black, S., Bell, F., Fothergill, R., Mellett-Smith, A., Jackson, M., McClelland, G., Gowens, P., Spaight, R., Igbodo, S., Brown, M., & Williams, J. (2024). The COVID-19 ambulance response assessment (CARA) study: a national survey of ambulance service healthcare professionals’ preparedness and response to the COVID-19 pandemic. British Paramedic Journal [online], 8(4), pp.10-20. Available at: https://doi.org/10.29045/14784726.2024.3.8.4.10
Belk, S., Armstrong, J., Ilczak, T., Webster, C. A., & Sumera, K. (2024). Student paramedic exposure to workplace violence: a scoping review. Critical Care Innovations [online]. Available at: https://doi.org/10.32114/CCI.2024.7.1.34.48
Bell, S. (2025). Simulation-based assessment in the context of paramedic education: A scoping review. The Clinical Teacher [online], 22(1), e13834. Available at: https://doi.org/10.1111/tct.13834
Bretherton, C. P., Hirst, R., Gacaferi, H., Gower, J., Exell, L., Johnston, S., Martin, S., Leech, C., Hilton, C., Battle, C., Axelrod, D., Vallier, H., Van Embden, D., Stockton, D. J., Cole, E., Williams, J., Johnson, L., Laubscher, M., Webb, Braude, P., Norris, S., Bell, S., Maqungo, S., & Griffin, X. L. (2024). Research priorities for the management of major trauma: an international priority setting partnership with the James Lind Alliance. BMJ open [online], 14(5), e083450. Available at https://doi.org/10.1136/bmjopen-2023-083450
Couper, K., Ji, C., Deakin, C. D., Fothergill, R. T., Nolan, J. P., Long, J. B., Mason, J. M., Michelet, F., Norman, C., Nwankwo, H., Quinn, T., Slowther, A.-M., Smyth, M. A., Starr, K. R., Walker, A., Wood, S., Bell, S., Bradley, G., Brown, M., Brown, S., Burrow, E., Charlton, K., Claxton A., Dra’gon, V., Evans, V., Falloon, J., Foster, T., Kearney, J., Lang, N., Limmer, M., Mellett-Smith, A., Miller, J., Mills, C., Osborne, R., Rees, N., Spaight, R.E.S., Squires, G.L., Tibbetts, B., Waddington, M., Whitley, G.A., V. Wiles, J., Williams, J., Wiltshire, S., Wright, A., Lall, R., & Perkins, G.D. (2025). A Randomized Trial of Drug Route in Out-of-Hospital Cardiac Arrest. The New England journal of medicine [online], 392(4), pp336-348. Available at: https://doi.org/10.1056/NEJMoa2407780
Couper, K., Ji, C., Lall, R., Deakin, C. D., Fothergill, R., Long, J., Mason, J., Michelet, F., Nolan, J. P., Nwankwo, H., Quinn, T., Slowther, A. M., Smyth, M. A., Walker, A., Chowdhury, L., Norman, C., Sprauve, L., Starr, K., Wood, Bell, S., Bradley, G, Brown, M., Brown, M, Charlton, K., Coppola, A., Evans, C., Evans, C, Foster, T., Jackson, M., Kearney, J., Lang, N., Mellett-Smith. A., Osbornre, R., Pocock, H., Rees, N., Spaight, R., Tibbetts, B., Whitley, G.A., Wiles, J., Williams, J., Wright, A., & Perkins, G. D. (2024). Route of drug administration in out-of-hospital cardiac arrest: A protocol for a randomised controlled trial (PARAMEDIC-3). Resuscitation Plus [online], 17, 100544. Available at: https://doi.org/10.1016/j.resplu.2023.100544
Fahmi, A., Palin, V., Zhong, X., Yang, Y. T., Watts, S., Ashcroft, D. M., Goldacre, B., MacKenna, B., Fisher, L., Massey, J., Mehrkar, A., Bacon, S., Hand, K., & van Staa, T. P. (2024). Evaluation of the impact of COVID-19 pandemic on hospital admission related to common infections: Risk prediction models to tackle antimicrobial resistance in primary care. PloS one [online], 19(12), e0311515. Available at: https://doi.org/10.1371/journal.pone.0311515
Holmes, E., Dixon, P., Mathieson, A., Ridsdale, L., Morgan, M., McKinlay, A., Dickson, J., Goodacre, S., Jackson, M., Foster, D., Hardman, K., Bell, S., Marson, A., Hughes, D., & Noble, A. J. (2024). Developing an alternative care pathway for emergency ambulance responses for adults with epilepsy: A Discrete Choice Experiment to understand which configuration service users prefer. Part of the COLLABORATE project. Seizure [online], 118, pp. 28-37. Available at: https://doi.org/10.1016/j.seizure.2024.04.008
Lunn, J., Brennan, L., Brewster, L., Hindocha, A., Patel, P., Stowell, C., & Isba, R. (2025). Burnout and staff experiences of health inequalities in children’s hospitals: a qualitative analysis. BMJ open [online], 15(2), e095418. Available at: https://doi.org/10.1136/bmjopen-2024-095418
Mercer, J., Morgan, D., & Lotto, R. (2024). A qualitative exploration of the views of paramedics regarding the use of dark humour. British Paramedic Journal [online], 9(3), pp. 37-43. Available at: https://doi.org/10.29045/14784726.2024.12.9.3.37
Noble, A. J., Dixon, P., Mathieson, A., Ridsdale, L., Morgan, M., McKinlay, A., Dickson, J., Goodacre, S., Jackson, M., Morris, B., Hughes, D., Marson, A., & Holmes, E. (2024). Developing feasible person-centred care alternatives to emergency department responses for adults with epilepsy: a discrete choice analysis mixed-methods study. NIHR Health and Social Care Delivery Research [online], 12(24), 1-158. Available at: https://doi.org/10.3310/hkqw4129
Noble, A. J., Lane, S., Lloyd, P., Morris, B., Bell, S., Shillito, T., Dixon, P., & Marson, A. G. (2024). ‘Blue-lighting’ seizure-related needs in care homes: a retrospective analysis of ambulance call-outs for seizures in North West England (2014-2021), their management and costs, with community comparisons. BMJ open [online], 14(11), e089126. Available at: https://doi.org/10.1136/bmjopen-2024-089126
Noble, A. J., Morris, B., Dixon, P., Mathieson, A., Ridsdale, L., Morgan, M., Dickson, J., Goodacre, S., Jackson, M., Hughes, D., Marson, A., & Holmes, E. (2024). Service users’ preferences and feasibility – which alternative care pathway for adult ambulance users achieves the optimal balance? Workshops for the COLLABORATE project. Seizure [online], 118, pp. 17-27. Available at: https://doi.org/10.1016/j.seizure.2024.04.010
Contact details
If you have any questions or concerns after reading this report, please contact us via e-mail: [email protected]
Should you wish to access any of our publications mentioned in this Quality Account, they can be accessed on our website at: www.nwas.nhs.uk