1. Chief executive’s statement
I am pleased to introduce the annual Quality Account for 2022/23. This document sets out the work we have delivered over the past year to improve the quality of our care, keep our patients safe and ensure staff wellbeing. It also provides information on our key priorities for 2023/24.
This has been another challenging year for North West Ambulance Service (NWAS), and, like other NHS organisations, we experienced unprecedented demand for all our services during the winter months. Despite this, we have continued to progress with improvements and led regional and national efforts to improve urgent and emergency care with our partners.
I want to acknowledge the contribution of the whole of NWAS to the body of work presented in this Quality Account and thank them wholeheartedly for their continued professionalism and commitment to the services we provide for our population in the North West. I would also like to thank our partner agencies, such as policing, fire and rescue, North West Air Ambulance, the military, third-sector partners, private ambulance providers and our volunteers for their unwavering support this year.
During 2022/23, we have published a new strategy which describes our core purpose ‘to help people when they need us most’ and our strategic objectives describe how we will deliver in the next three years. Our safety and quality ambitions are implicit within our organisational strategy and build on our Quality Strategy, which will be re-launched in 2023/24.
The context we operate in has seen significant change in the last year. Our longstanding relationships with clinical commissioning groups (CCG) have been replaced with place-based leadership under the governance of the integrated care boards (ICB). Likewise, our provider colleagues have coalesced into provider collaboratives and primary care networks. The changes in our landscape have required us to re-establish relationships and work on new governance arrangements aligned with this emergent system governance. We have
strengthened our management and reporting structures to align with the integrated care systems (ICS) footprints.
We have also worked with colleagues in NHS England (NHSE) and the Care Quality Commission (CQC) to build strong relationships with the local regulators. We have also built on the inspection of our 111 and 999 services as part of the urgent and emergency system inspections in South Cumbria and Lancashire and Mersey North which reported out in this financial year and resulted in us retaining our overall rating of GOOD.
We have made real progress in the delivery of our 2022/23 goals – highlights include:
- Significant progress with our patient safety programme by recruiting patient safety partners, preparing to implement the national Patient Safety Incident Response Framework (PSIRF) and working to better understand safety culture in high-risk settings such as our control centres.
- Working with system partners to improve urgent and emergency care service responsiveness via a North West hospital handover collaborative.
- Partnering with mental health providers and policing to work differently in our control centres to provide an enhanced response for patients presenting to 999 services in mental health crisis.
- Implementing a new incident reporting system to enable more scrutiny of harm
Datix Cloud IQ (DCIQ).
- Significant steps to align our 999 and NHS 111 call triage systems, using NHS Pathways in both operational environments.
- Sustained high performance in 999 call handling to respond to patients when they call.
- Significant improvements in hear and treat rates to ensure patients receive the right care when they call.
I have continued to provide leadership for the ambulance sector as a whole as Chairman of the Association of Ambulance Chief Executives (AACE). This has put NWAS at the forefront of thought leadership for the ambulance sector.
I feel an overriding sense of immense pride in how hard everyone has worked and continues to do so. Without doubt, every member of staff and our volunteers stepped up during this period to ensure that, despite the situation, we could continue to provide the best possible service to our patients. I want to thank every staff member and volunteer for their outstanding efforts.
Daren Mochrie QAM, MBA, Dip IMC RCSEd, MCPara Chief Executive Officer
- Statement of directors’ responsibilities in respect of the Quality Account Under the Health Act 2009, National Health Service (Quality Accounts) Regulations 2010 and National Health Service (Quality Account) Amendment Regulation 2011, the directors must prepare quality accounts for each financial year. The Department of Health has issued guidance on the form and content of annual quality accounts (which incorporate the above legal requirements).
In preparing the Quality Account, directors must take steps to satisfy themselves that:
- The Quality Account presents a balanced picture of our performance over the period covered.
- The performance information reported in the Quality Account is reliable and accurate.
- There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice.
- The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review, and the Quality Account has been prepared in accordance with Department of Health guidance.
The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account.
By order of the Board
2. Overview
North West Ambulance Service (NWAS) is one of the largest ambulance trusts in England. We provide services to over seven million people across a geographical area of approximately 5,400 square miles. We employ 7,079 staff from over 100 sites and provide services to patients in rural and urban communities, coastal resorts, affluent areas and in some of the most deprived inner-city areas in the country. We also provide services to a significant transient population of tourists, students and commuters. The North West region is one of England’s most culturally diverse areas, with over 50 languages spoken by community members. Consequently, we place considerable emphasis on equality and diversity and public engagement activities to ensure that our services are accessible to all members of the community.
People living in our communities are sicker than before the Covid-19 pandemic. They have been hesitant to access health services and others have waited a long time for some conditions to be diagnosed and treated. There are more people living with long-term conditions and, as people get older, we can expect there will be more people in our communities living with illnesses. We know from our data that the overall health of our
region’s population has an impact on demand for our services. If we can address the health inequalities within the North West and help tackle the causes of illness by looking at the wider factors that affect our health, we can help people to stay healthy and reduce the need for them to have care from the NHS.
This year a strategic focus for NWAS has been the opportunity to work in partnership with the integrated care systems (ICS) and newly formally integrated care boards (ICB) to support the delivery of public and population health agendas and urgent and emergency care pathways. From 1 July 2022, integrated care boards became statutory bodies. ICSs have brought together commissioners of NHS services with health and care providers and other partners who work together to deliver services which meet the needs of specific populations. We are the only regional NHS organisation in the North West that operates across five ICSs:
- Lancashire & South Cumbria Health & Care Partnership
- Cheshire & Merseyside Health & Care Partnership
- Greater Manchester Health & Social Care Partnership
- North East & North Cumbria ICS
- Joined Up Care Derbyshire (which includes Glossop)
While there are challenges with working across many ICS areas, we have gained experience as a key partner within the urgent and emergency care (UEC) system. We deliver services across a large area and have valuable data and insight which helps to identify opportunities for improvement, share learning and best practice. During 2022/23 we have been working with system partners across the North West to deliver a hospital handover collaborative.
The future of integration needs health and care providers to work alongside patients to design services around people’s needs, with a focus on preventing serious health problems and reducing health inequalities. We have an opportunity to work together within our ICSs to support this work and help people when they need us most.
To fully participate and be engaged with stakeholders, we have continued to progress system collaboration in achieving shared goals, enhancing our role as a proactive, trusted partner.
2.1 Vision and aims
At NWAS, everyone is connected by a shared purpose; to help people when they need us most. We aim to achieve the best possible physical and mental health outcomes for each person who needs us. We will provide high-quality emergency care to save lives and make a difference to people with life threatening illnesses or injuries. For those with less serious conditions, we will tailor our response to each person’s needs. This may include urgent clinical assessment, advice over the phone, referring them elsewhere or alternative transport for scheduled appointments.
Our vision is to deliver the right care, at the right time, in the right place; every time. Each element of our vision has a clear definition:
- Right care means that we will provide outstanding care that is safe, effective and focused on the needs of the patient.
- Right time means that we will achieve all operational performance standards for our paramedic emergency service, NHS 111 and patient transport service.
- Right place means that we will provide care in the most appropriate setting for each patient’s needs, taking fewer people to emergency departments by providing safe care closer to home or referring people to other health and care pathways.
- Every time means that we will provide services which are consistent, reliable and sustainable.
To deliver our vision, everyone at NWAS is expected to embody our values of working together, being at our best and making a difference. Our values guide the behaviours that underpin all that we do; putting our values into practice supports us to provide compassionate care and improve outcomes and experiences for our people, patients and communities.
Our 2022-2025 strategy
In the financial year of 2021/22, we began an ambitious programme of work to review and rewrite our strategy. Extensive work was completed to understand what staff, volunteers, patients and service users felt was important for us to focus on over the next three years. Our new strategy aims and objectives were approved in May 2022. There are three main aims, with the first one related to quality. These are set out below, and this Quality Account further details specifics for the first aim, ‘to provide high quality inclusive care that is safe, effective and person centred’ is contained within this Quality Account. Details and specifics related to aims two and three are included within complementary documents including the NWAS Annual Report 2022/23 and the NWAS Equality, Diversity and Inclusion Annual report 2022/23.
Strategic aims
Our three, organisational aims give a framework of what we will focus on between 2022- 2025 to achieve our vision.
Aim 1: Provide high-quality, inclusive care
We recognise there are health differences between groups in the communities we serve. We will listen, to understand and make sure our services are accessible to everyone. We will work to prevent harm while using learning and research to continuously improve patient care and experience. To achieve this aim, we must create the conditions to provide care which is:
- Safe
- Effective
- Person-centred
Aim 2: Be a brilliant place to work
We will create an environment where our people feel happy and safe, have access to equal opportunities and are supported to be at their best. We will be a brilliant place to work by:
- Looking after our people
- Investing in our people
- Leading our people compassionately
Aim 3: Work together to shape a better future
We will work together to improve the services we provide. We will work with our partners and the public to find solutions which improve access, outcomes and experience for everyone. We will work together to become more sustainable and positively affect our communities and environment. To deliver this aim, we will work together, internally, with partners across the North West, and with communities to work towards:
- One NWAS
- One North West
- One future
3. Our services
NHS 111: deliver 111 services for the North West region and are major contributors to the delivery of integrated urgent care. We signpost patients to the most appropriate care highlighted to them following triage and informed by the Directory of Services.
Emergency Operation Centre (EOC): receive and triage 999 calls from members of the public as well as other emergency services. EOC staff provide advice and dispatch an ambulance service to the scene as appropriate. The Clinical Hub (CHUB) is based within the EOC and assesses patients via telephone and provides the most appropriate care based on that assessment, known as hear and treat. This may be an ambulance (either emergency or urgent care), GP referral, referral to other services or self-care.
Paramedic Emergency Service (PES) or 999; solo responders, double crewed ambulances and volunteer community responders who provide emergency care to 999 and urgent calls for the population of the North West.
Resilience: Our hazardous area response team (HART) and resilience teams are specially trained and equipped paramedics to provide ambulance response to high-risk and complex emergency situations, including major incidents. They respond to major incidents to deliver our statutory responsibilities as a Category 1 responder under the Civil Contingencies Act 2004.
Patient Transport Services (PTS): provide essential transport to non-emergency patients in Cumbria, Lancashire, Merseyside, and Greater Manchester, who are unable to make their own way to or from hospitals, outpatient clinics or other treatment centres.
Corporate services: As well as providing clinical services to patients, we provide a wide array of specialist, non-clinical corporate services. These wider teams offer a unique variety of services, for example; estates and facilities, communications, risk management, digital, vehicle maintenance, finance, and human resources.
Volunteering: we have one of the largest and longest-established community first responder (CFR) schemes in England, with some 567 active CFRs operating across all areas
of the North West, providing an effective, complementary service in their local communities. CFRs are volunteers who live and work in local communities. They are trained and activated by our emergency operations centre to attend certain calls, such as chest pain or cardiac arrest, where time to respond is critical and can make the difference between life and death. CFRs provide care and support to the patient until the arrival of an emergency ambulance. All responders are equipped appropriately to respond to the emergency they are sent to, they have access to the required levels of personal protective equipment (PPE) for their skill set and we continually review this to ensure it fits with both organisational and national requirements.
Patient transport volunteer car drivers also play an invaluable role in transporting patients to and from hospital appointments which include renal dialysis, oncology and routine appointments. The 190 operational volunteers operate across the North West and transport patients in their own vehicles whilst offering a friendly face and listening ear by putting patients who are often anxious or concerned about their appointment at ease.
We also have volunteers involved in our Patient and Public Panel. The panel has gone from strength to strength, and we now have 268 members. A focus for 2022/23 has been to increase the diversity of the panel to represent all the communities across the North West.
4. Operational performance
Section four of the Quality Account summarises operational performance and service delivery achievements during 2022/23.
4.1 NHS 111
In 2022/23, NHS 111 call demand continues to be consistent over the year. However, there have been periods of volatility based on external factors, for example Covid-19 and Strep A. The high-level publicity of the outbreak of Strep A, meant a significant unplanned increase in call volume in quarters 3 and 4 of 2022/23 seeing a rise in volume of over almost 36,000 more calls compared to the previous year.
Performance standards
Calls answered key performance indicator (KPI) 95% within 60 seconds, increased from an average of 18.75% in 2021/22 to 36.85% in 2022/2023. Calls abandoned KPI <5% averaged at 23.1% in 2021/2022. This year saw a decrease to 17.5% during 2022/23.
Performance standards were:
| Description | Target | Year | Q1 | Q2 | Q3 | Q4 |
| Calls abandoned | <5% | 2021/22 | 14.21% | 27.61% | 28.07% | 22.54% |
| 2022/23 | 18.84% | 10.53% | 28.38% | 17.25% | ||
| Calls answered in 60 seconds | 95% | 2021/22 | 47.52% | 28.45% | 29.32% | 33.84% |
| 2022/23 | 34.90% | 51.40% | 32.20% | 28.90% | ||
| Calls warm transferred | 75% | 2021/22 | 19.23% | 15.08% | 12.54% | 12.16% |
| 2022/23 | 15.80% | 17.20% | 10.60% | 22.00% | ||
| Callbacks within 10 minutes | 75% | 2021/22 | 5.49% | 4.87% | 4.71% | 6.49% |
| 2022/23 | 7.40% | 9.70% | 7.60% | 8.80% | ||
| Calls Offered | N/A | 2021/22 | 710,638 | 703,167 | 719,285 | 583,475 |
| 2022/23 | 612,253 | 545,863 | 727,214 | 611,481 | ||
| Calls Answered | N/A | 2021/22 | 558,347 | 459,831 | 458,890 | 395,970 |
| 2022/23 | 454,842 | 441,242 | 453,204 | 396,096 |
Table 1: 111 Performance Standards 2022/23
During 2022/23 the following service delivery improvements were undertaken:
111 Development Forum: This meeting is held every six weeks and offers staff the chance to hear about and discuss any developments ongoing or upcoming, including system changes. Staff can make suggestions to the forum around improving any aspect of 111. The meeting is now well embedded within 111 and is always extremely well attended by staff from across the service line. Many of the developments we make come out of suggestions to the group.
Care advice by SMS (Text message): Following a trial of sending patients care advice by SMS instead of verbalising the advice, 111 have fully implemented this service. The work has been recognised nationally and 111 presented the project results to a 111 providers forum hosted by NHS Pathways. The presentation was well received, and several providers have contacted us since the meeting for more information. As a result of this work, the triage time for calls where the patient receives their care advice by SMS takes 29% less time than similar calls where the care advice is delivered verbally.
Directory of Service (DoS) Review Group: The Directory of Services is a repository of local services, populated and kept up to date by local commissioners, that the 111 system will interrogate following triage to find suitable local services to support a caller’s need. The Directory of Service task & finish group was created to reduce the number of healthcare professional feedback forms submitted to 111 and was successful in that aim. As the group was still considered valuable by members, the task and finish group has now become the Directory of Service review group. This meeting has strengthened relationships with colleagues from regional and local Directory of Service teams. We continue to discuss ways we can improve the Directory of Service and the way it is used in 111 as well as monitoring healthcare professional feedback as a way of highlighting any areas of concern or potential for improvement.
OneSpace: The 111 SharePoint site was recently rebranded as OneSpace. The site is extremely well used, with consistently over 20,000 monthly hits from over 700 individual users. As well as being a single point of access for communications within the department and standard operating procedures, the site continues to develop with specific pages for the resource and planning team, Directory of Service team, industrial action planning and NHS Pathways as well as information about staff development and health and wellbeing. Further development is planned, including specific pages for the systems and quality and assurance teams.
Pathways release updates: NHS Pathways is the triage system utilised by all NHS 111 services and half of the English ambulance service providers to triage calls. Regular updates are released every eight weeks. The process of training and releasing these updates is a standard part of business as usual in 111. As our emergency operations centre call handlers now triage calls using NHS Pathways, we have taken the opportunity to ensure a consistent approach by regularly meeting to share progress and learning as well as ensuring that our updates are completed together to ensure that callers always receive the same triage regardless of whether they call 111 or 999. This work will again make future integration of service lines more straightforward.
Direct booking report: It is crucial to have two-way communication with the broader healthcare system as the 111 provider for the North West. One of the ways that we maintain that communication is through a monthly report that details appointments and bookings of different types across the four ICBs in the North West. The report has had a recent design change in mid-late 2022, driven by feedback and the desire to improve the quality of our work consistently. It is used widely across ICBs and shared with key stakeholders across the North West.
Advisor reading time: In response to staff feedback through the development forum and learning forum, call handling staff now receive five minutes offline time up to three times a week. This allows them to keep on top of important communications on OneSpace and email.
Cardiopulmonary resuscitation (CPR) training: Completion of CPR workshops to increase staff confidence with delivering instructions via telephone. This saw a decrease in time from the start of triage to the start of CPR commencing. Plans to further the improve the start of call to start of CPR to introduce questions around consciousness and breathing at the start of the call to prevent unnecessary delay in providing advice.
Clinical queue task group: The purpose of this work is to evaluate and implement changes which reduce the number of cases being placed in the queue unnecessarily. This aims to improve the patient journey by directing callers to the appropriate place of care at the point of the call and reduce to need to wait extended periods to receive a call back which doesn’t
add value to the patient.
Visual Interactive Voice Response: 111 has designed an improvement to the current Interactive Voice Response (IVR) to allow patients who call 111 using a mobile phone to opt in to complete their demographic information using their phone when the wait time is sufficiently long enough. When this takes place and the call is answered, the demographic information is automatically presented to a health advisor including a personal demographic service (PDS) trace where possible. This will reduce the time from call answer to triage start significantly and will increase the number of calls 111 can answer as well as improving the patient experience by reducing the time to triage for these patients.
Cleric digital alerts: Within the 111 contact centre, advisors sometimes require extra help when they are speaking to patients. In the past, when help was required, an advisor would raise a physical card to attract the attention of a shift manager. After a suggestion from the 111 development forum, we developed a system for raising and acknowledging alerts within Clerics. This innovation came from within the contact centre itself. The process of the development forum and other groups allowed for this idea to come to life.
Improved patient location services: To improve the location of callers to 111 and based on a suggestion from the 111 development forum we have implemented the use of two precise location services, What3Words and CCS locations. We now can locate patients by asking them for their What3Words details or by sending them an SMS with a link to provide their location. This information is useful if the patient requires an ambulance response, and it is not at their usual place of residence.
Health Advisor Hybrid working (Azure Virtual Desktop):111 have been working closely with our IT team to roll out a new virtual desktop solution to allow health advisors to take incoming calls whilst working from home. The first live call was taken on the 19 January 2023. The Azure Virtual Desktop system continues to be developed by our IT team and further homeworking trials are planned to allow more Health Advisors to adopt hybrid working.
Booking and Referral Standard (BaRS): A patient journey, from the patient presenting with symptoms, to appropriate treatment then discharge, often involves two or more NHS services. Booking, clinical and administrative information need to follow the patient at all stages of this journey. This frequently requires paper processes and multiple healthcare IT systems, which can be inefficient. To help solve this problem, we have implemented a new booking and referral standard (BaRS). It ensures healthcare professionals receive the information they need, in a format they can use, integrated into their existing healthcare IT systems. 111 have implemented BaRS between 111 and Warrington ED and Halton/Runcorn urgent treatment centres as the first of type nationally. Testing was completed, and we went live with BaRS on 28 February 2023. This is a major milestone for our 111 service and involvement in this project has been recognised nationally. BaRS will continue to be developed to be used across the Emergency and Urgent Care system.
Staff welfare improvements implemented during 2022/23 include:
111 Champions: These roles have continued to support the health and wellbeing of the call centre staff, being recognised by being awarded the making a difference award at our annual Star Awards event. They continue to organise health and wellbeing events to encourage good health and support to each other. They are a positive influence within the contact centres.
Employee of the month: This initiative was introduced to help recognise excellence within the call centre.
111 rota review: In August 2022, 111 began a rota review. The previous rota review took place in 2019 and, since then, several changes have affected 111. As a result of the Covid-19 pandemic and 111 First, demand has changed significantly. 111 are receiving more calls and at different times of the day. This means that we are seeing patients waiting to be answered more often than before. The rota review will help align staff to better rotas, making patients much safer by answering our calls much sooner.
4.2 Emergency Operation Centre
During 2022/23, the Emergency Operation Centre, Clinical Hub (CHUB) and 111 services began to integrate, with the long-term goal being full integration of the respective services line into Integrated Contact Centres. The primary focus for this year has been to integrate governance and senior leadership reporting under the integrated contact centre director.
The primary enabler of integration has been the introduction of NHS Pathways within the EOC. The programme to move from Medical Priority Dispatch System (MPDS) triage tool to NHS Pathways has been a long-standing strategic ambition, fully realised during 2022/23. With both service lines operating on the same primary triage tool there is greater scope to integrate front line and management roles. This will be the strategic focus for 2023/24. The move to NHS Pathways has provided several key benefits for contact centres and for ARP performance. In terms of contact centres these benefits include:
- Patients now receive the same outcome, treatment, or referral appropriate to their clinical need, irrespective of the number dialled (i.e. 111 or 999).
- Enhanced and closer working of the respective service lines.
- Integration of clinical and leadership governance and structures.
- Ability to flex workforce across the respective service lines to meet peaks in demand and operational pressures.
The contact centres have commenced this journey and already utilised these benefits. As an example, during quarter 3, the demand faced by the 999 element of the service continued to increase, creating delays in calls being answered and sending a response to high acuity patients. This new way of working allowed the team to test a dual call handling approach.
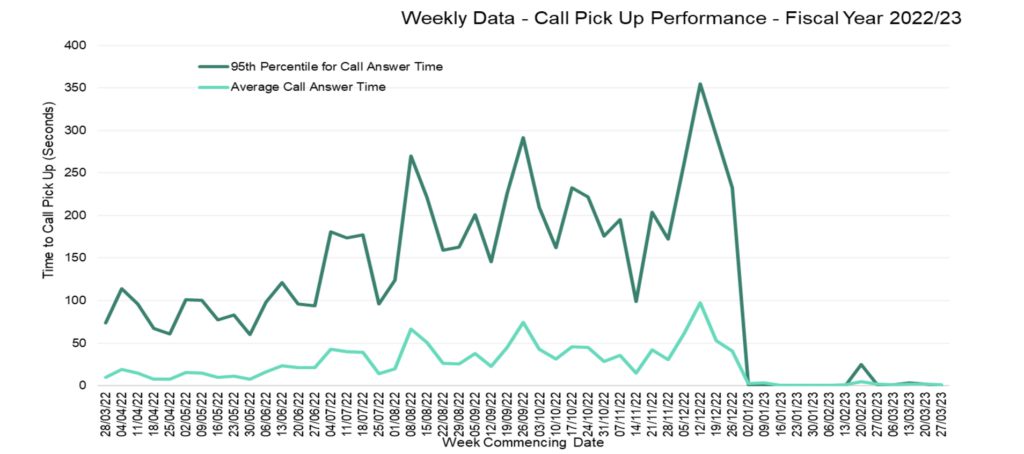
This resulted in 111 Health Advisors moving across to the EOC environment to answer 999 calls and mitigate the risks associated with delayed call answering. Figure 1 below shows the weekly average time to answer calls against the national standards set during 2022/23.
In terms of the benefits of NHS Pathways in respect to ARP response, the programme has delivered on these from the outset of go live. These benefits include:
Reduction in the proportion of Category 1 and Category 2 incidents: Quarter 4 data 2022/23 reflects a Category 1 percentage of incidents at 9.43% against a 2021/22 annual position of 13.71% (a reduction of 31%). This finer triage ensures those patients presenting with immediate life-threatening presentations, and require multiple resources to be dispatched are identified, whilst correctly identifying those that do not need multiple resources previously identified by MPDS, thus freeing up more resources to respond to other 999 calls. This is due to the triage mechanism and application of NHS Pathways.
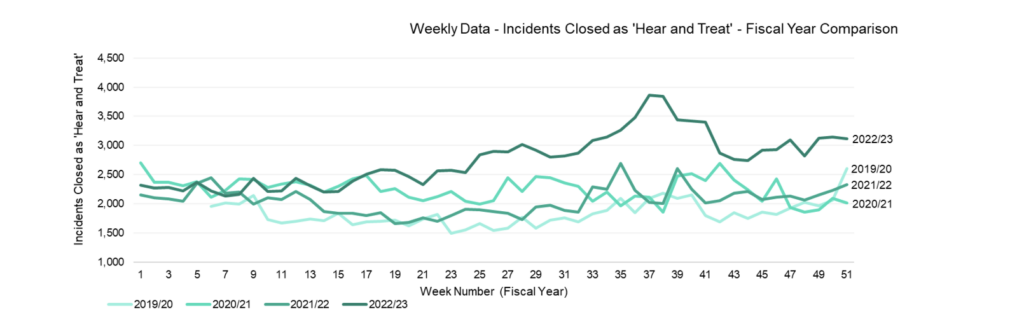
Increase to hear and treat: NHS Pathways provides a level of hear and treat, when a call is triaged and it is identified that a local service is more suitable to support the patients need rather than dispatching an emergency ambulance, via the call handlers within the EOC. The previous triage tool MPDS did not provide this. Around 5% of all call triaged via NHS Pathways result in a call handler hear and treat where the patient is referred via the Directory of Service to the appropriate care setting (often primary care, urgent treatment centres or emergency departments).
Programme benefits: Overall the programme outlined 25 strategic benefits (5 of which are long term benefits relating to integration of the service lines).
Emergency Operation Centre and Clinical Hub highlights
We have been able to continue investment within Emergency Operation Centre and Clinical Hub (CHUB) throughout the challenging period felt by the NHS in 2022/23. Extra funding received from commissioners and NHS England from Covid-19 and winter monies have enabled us to recruit extra staff to respond to the increase in 999 call activity over this period and increase the call handling establishment to ensure 999 calls are answered in a timely manner against national targets. The benefit of this was realised in quarter 4 of 2022/23 with us achieving both national standards for this quarter, with zero seconds for the 90th centile target and 2 seconds from the mean target.
We also continued to enhance patient safety and clinical leadership across our contact centres. The CHUB have increased their workforce position delivering increased hear and treat and greater capacity to support the Clinical Coordination Desk in reviewing patients that may have waited longer than was expected to reduce the risk of potential harm.
Other summary highlights for EOC and CHUB include;
Integration of the Reginal Trauma Cell into the Complex Incident Hub, giving a better process of managing and deploying our specialist recourses, and having an increased situational awareness of developing incidents across the whole north west footprint.
The Clinical Coordination Desk has seen an increase and development in its function and ability to manage the potential risks of patients waiting longer for an ambulance response because of high demand at the time and give crew clinical support and advice when required.
Introduction of the direct to dispatch recruitment, the benefit of this is that we are not just recruiting from existing staff and therefore reducing that pool of experienced staff, and this means we are bringing in a whole new cross section of knowledge and experience into dispatch.
Audits of dispatch of ambulance resources was introduced in 2022/23 for Category 1 calls, to ensure that the correct resource has been allocated to incidents, to reduce missed allocation opportunities. The audit has been reported to the Commissioner led Regional
Clinical Quality Assurance Committee showing 95% compliance and has started for Category 2 calls with the intention to continue this to include further category of calls. Our Support Centre has now moved to utilising the Cleric system to send electronic referrals for safeguarding concerns and patients identified as at risk of falls into suitable local services to support these patients. Using Cleric will lead to a more robust system for escalating high-risk patients within those categories to the relevant service and give consistency across the service lines.
The Clinical Hub is developing and building on a hybrid working model, allowing staff to perform remote telephone triage and face to face assessment within the same shift, increasing effectiveness, autonomy, and job satisfaction, whilst delivering the most appropriate care for the patient.
4.3 Paramedic Emergency Services
The number of 999 calls received in 2022/23 reduced to circa 1,697,000 when compared to some of the sustained high numbers in 2021/22, circa 1,808,000 as illustrated below.
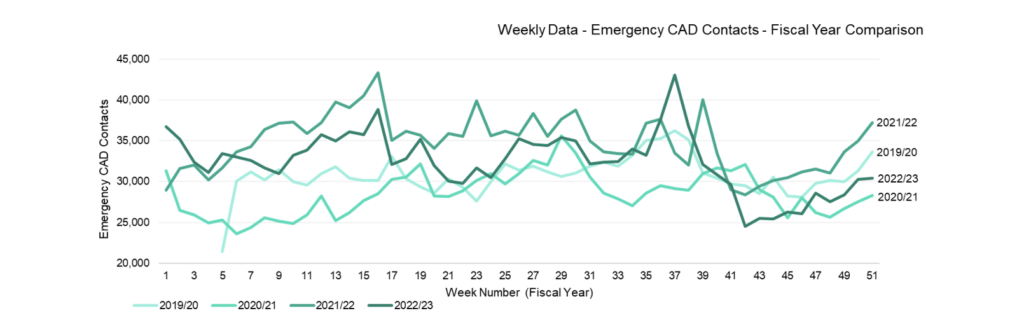
However, 999 call demand in quarter 3 2022/23 was extremely challenged compared to previous years for the same period, resulting from a peak in respiratory illness associated with influenza and was further impacted by periods of industrial action in our service and other NHS partners.
In 2022 we introduced NHS Pathways as a front-end triage system to the 999 service to align to 111 where we have been using the system for some time. This work has exceeded our
year one expectations and has enabled the clinically safe signposting of patients at the time of their first call or following clinical reassessment callbacks. The proportion of 999 calls now closed with telephone advice or onward referral, and therefore with no requirement for an emergency ambulance to be dispatched, has been exceeded 15% during quarter 4 2022/23. This vital change in systems has very clear benefits for patients in either gaining the right care sooner from local services closer to home, or receiving an ambulance response more reliably as this will increase the availability of ambulances to respond in a more timely and efficient manner.
Ambulance Response Programme
NHS England set the performance targets for English ambulance services in 2017, known as the Ambulance Response Programme (ARP) standards. This system requires triaged calls needing an ambulance response to be placed in four category types, depending on the acuity and need of the patient. These categories then have response times allocated to them under the standards, which are appropriate for the patient’s presentation at time of call, as listed below:
- Category 1 – 7 minutes mean and 15 minutes for 90th centile
- Category 2 – 18 minutes mean and 40 minutes for 90th centile
- Category 3 – 120 minutes for 90th centile
- Category 4 – 180 minutes for 90th centile
As demonstrated in the table below, during 2022/23 we found the response times challenging, especially during quarter 3, when we felt extreme pressures, along with many NHS systems across the country. Following the quarter 3 2022/23 challenges, we have seen some recovery in quarter 4 2022/23.
| Standard | 7 mins | 15 mins | 18mins | 40 mins | 120 mins | 180 mins |
| Q1 | 00:08:14 | 00:14:01 | 00:40:09 | 01:29:18 | 07:15:31 | 11:46:07 |
| Q2 | 00:08:27 | 00:14:28 | 00:41:41 | 01:33:38 | 08:03:43 | 09:57:53 |
| Q3 | 00:09:25 | 00:16:03 | 00:58:12 | 02:09:09 | 10:36:47 | 12:40:03 |
| Q4 | 00:08:17 | 00:14:06 | 00:27:50 | 00:58:18 | 04:33:48 | 06:29:01 |
| 2022/23 | 00:08:39 | 00:14:45 | 00:45:04 | 01:42:14 | 07:25:41 | 12:27:24 |
| 2021/22 | 00:08:42 | 00:14:48 | 00:47:39 | 01:47:54 | 07:09:45 | 14:27:14 |
It is important to note that the 2022/23 quarter 3 and quarter 4 periods included periods of industrial action directly and indirectly affecting us. Our planning and response to these periods maintained a high quality and safe emergency service throughout. This response could not have been delivered without a ‘one NWAS’ approach, including the training and deployment of additional military colleagues as part of a national Military Aid to Civil Authorities (MACA) mobilisation on several days between December and March, as well as mobilising additional private and voluntary emergency ambulance providers across all areas.
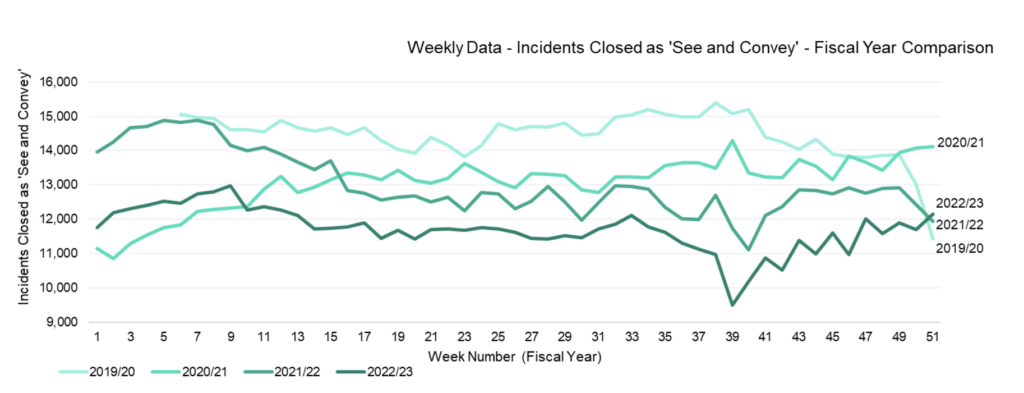
During 2022/23 we, alongside commissioners, ICBs and local services, continued to work towards ensuring all patients receive care closer to home whenever it is identified it is more appropriate than transporting to the emergency department (ED). This has included collaborative work with local two-hour urgent community response services, Same Day Emergency Care (SDEC) and mental health services to ensure patient calling 999 receive the right care for their need. In 2021/22 we conveyed around 684,500 patients to emergency departments, 57% of all incidents whereas in 2022/23 this was reduced to circa 539,500, 50% of all incidents.
We implemented in year tests of change to support patients with mental health crisis and falls without injury, as well as improving our technical connectivity for clinicians to make safe clinical referrals to community services electronically.
As seen in the graph below from week 9 of 2022/23, we transported less patient to hospital than in any previous year.
In 2022/23 the North West region’s health and social care system has also been under significant pressure. The impact this has seen for us is in delayed handover times across the region, which in turn can impact ambulance availability. Although nationally we have not been as challenged as some regions, it has still caused challenges for us in delivering ARP performance and responding to patients in the community.
To help systems improve their hospital handover times we mobilised local and regional handover collaboratives with ICB leads and hospital providers, to address this shared area of significant clinical risk. Work is underway to maximise conveyance to alternatives to emergency departments, including Same Day Emergency Care (SDEC) as well as connecting patients to ‘virtual wards’ as they expand in 2023/24. Virtual wards allow patients to get the care they need at home safely and conveniently, rather than being in hospital. Virtual wards are increasingly being introduced across the North West.
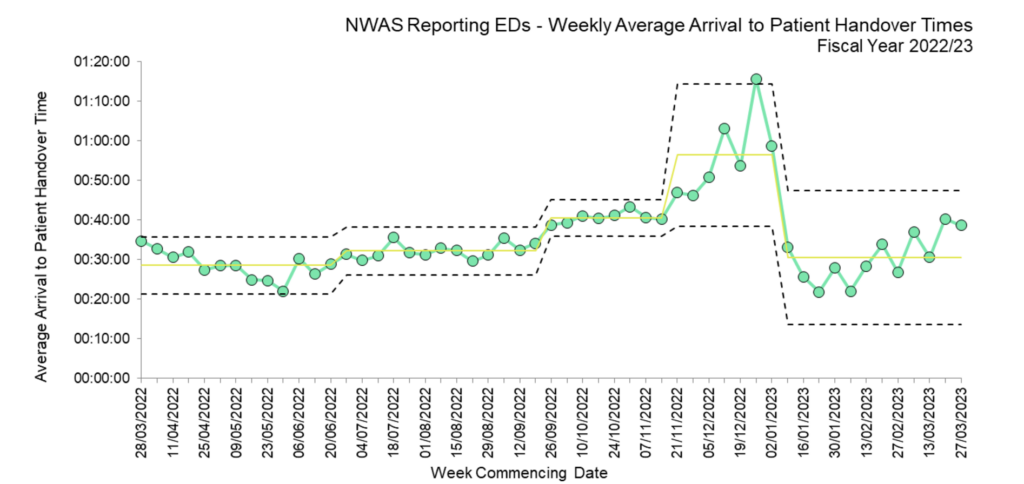
Our operational management teams have worked hard throughout the year to reduce variation in the time taken after handover to make vehicles ready to respond again. The predominant area of avoidable lost emergency ambulance time is in the arrival to handover period. Across the region we conveyed over 539,500 patients to hospital and lost over 123,000 hours of emergency ambulance time to handovers taking longer than the 15- minute target. Figure 5 below demonstrates the upward trend in average arrival to handover during the year, and the extreme challenges presented to us during quarter 3 2022/23, which has recovered to a much-improved position by the year end, though that improved position remains far higher than the 15-minute standard.
4.4 Resilience
Our contingency planning arrangements and capabilities assist in providing evidence of compliance with our duties under the Civil Contingencies Act (CCA), 2004, the Health and Social Care Act 2008, Regulations 2010 and the NHS England Emergency Preparedness, Resilience and Response (EPRR) Framework together with other legislation such as the Corporate Manslaughter and Corporate Homicide Act 2007 and the Human Rights Act 1998.
The NHS needs to plan for, and respond to, a wide range of incidents and emergencies that could affect patient care or public health. The manifestations of this could be precipitated by a wide range of triggers from infectious disease, as with the current Covid-19 pandemic, transport emergencies, industrial incidents/action, infrastructures failures or terrorist attacks. The Civil Contingencies Act, 2004 requires all NHS organisations and providers of NHS funded care, to demonstrate that they can effectively respond to such incidents whilst maintaining core services.
Under the EPRR arrangements, all NHS trusts which are also designated Category 1 responders, such as ours, under the Civil Contingencies Act 2004, are required to undertake an annual, self-assessment process to determine the level of compliance of resilience arrangements measured against the NHS England (NHS) core standards.
EPRR annual assurance
As the NHS Core standards for EPRR provide a common reference point for all organisations, they are the basis of the EPRR annual assurance process. Providers and commissioners of NHS-funded services complete an assurance self-assessment based on these core standards. This assurance process is led nationally and regionally by NHS England and locally by Integrated Care Boards (ICB).
NHS England (NHSE) requires this assurance exercise to identify any areas of limited or no compliance (as well as highlighting areas of complete compliance) of resilience arrangements against the EPRR core standards, with any deficiencies in particular areas forming an individual action plan. This plan will demonstrate the intention of each trust to address any outstanding issues and give an indication of priority and timescale for resolution.
10 domains cover the NHS core standards for EPRR, with an 11th domain applicable only to the NHS ambulance trusts which covers interoperable capabilities they must have in place. A full review of the core standards is conducted every three years, which was conducted in 2022. This has seen an increase in the number of core standards that need to be assessed within the domains, as well as requiring PTS to be assessed for the first time as well as NHS 111 and the wider trust.
As part of the 2022/23 NHS Core Standards on the 24 October 2022 a submission on the EPRR Annual Assurance self-assessment which provided the following:
Rating definition
The EPRR assurance rating of “Substantially Compliant” represents 89-99% compliance,
“Partially Compliant” represents 77-88% compliance.
Core Standards: Out of 50 applicable standards, we have self-assessed full compliance with 45 and partial compliance with 5. This represents a compliance figure of 90% and therefore an overall rating of “Substantially Compliant”.
NHS 111 Standards: Out of 43 applicable standards, NHS111 have self-assessed full compliance with 36 and partial compliance with 7. This represents a compliance figure of 84% and therefore an overall “Partially Compliant” rating.
Patient Transport Standards: Out of 42 applicable standards, PTS have self-assessed full compliance with 35 and partial compliance with 7. This represents a compliance figure of 83% and therefore an overall “Partially Compliant” rating.
Interoperable Standards: Out of 163 applicable standards, we have self-assessed full compliance with 137 and partial compliance (including 2 non-compliant) with 24. This represents a compliance figure of 84% and therefore an overall rating of ‘Partially
Compliant’.
Special operations
The Special Operations discipline within resilience manages the following interoperable capabilities work streams.
- Hazardous Area Response Teams (HART)
- Special Operations Response Team (SORT)
- Chemical Biological Radiological and Nuclear (CBRNe) response
- Marauding Terrorist Attack (MTA) response
- Medical Emergency Response Incident Teams (MERIT)
- Command Training & Education
- Major Incident Fleet
- National Inter Agency Liaison Officers (NILOs) and Tactical Advisors
During 2022/23 the department was involved in various and wide-ranging projects. Specifically related to HART, was the completion in training of 290 staff as Special Operations Response Team operatives (SORT). This project commenced in 2021 led by one of the special operations’ senior leaders, planning and delivering 5 days training in the subject matter of CBRN and MTA. In addition, SORT operatives were also trained in driving
7.5 tonne vehicles and in on scene logging. This training and resource enhance the current capabilities of HART and all operational resources in responding to incidents, including those declared as a major incident.
Training and education is a core function with HART and in addition to supporting the SORT training the HART team delivered several other specialise training:
- High Risk Confined Space Rescue
- HART trained in High Risk Confided Space
- HART trained in the new PPE (NxGen)
- High Consequence Infectious Disease (HCID) including Epishuttle
Special Operations senior leadership team continue to work with stakeholders in developing a new HART site based in the Liverpool area, with a site identified and by the end of the financial year reached the planning stage.
The State Funeral of Her Majesty the Queen brought national and global attention, and we were proud to support the occasion through Special Operations. This was a proud moment and a memorable occasion.
From a clinical perspective, the HART clinical lead was heavily involved in the standardisation of HART skills nationally and agreeing to a training programme for HART Specialist Paramedics in the administration of Ketamine and front of neck airway access. The clinical leadership continues to strengthen its position working with senior clinicians across the medical directorate, and nationally.
MERIT continues to go from strength to strength with an establishment of 40 doctors who have all attended their annual training programme, with many attending monthly evening CPD sessions held to fit around their busy professional commitments. The Strategic Medical Advisor Cadre has also undertaken their annual training programme in support of the capabilities. MERIT have played a key role through several incidents response, and they have provided a key resource during periods of high demand, and through periods of Industrial Action. MERIT is a key resource providing senior medical response and support for our emergency workface at the scene on the frontline.
Annual Commander training continues throughout the year with the subject matter specific to CBRN. The annual commander training is mandatory for all Strategic, Tactical, Operational Commanders and National Interagency Liaison Officers (NILOs), EOC On Call and Duty Control Managers from the Emergency Operations Centre. Annual Commander training will continue through 2023/2024 however, significant work has been undertaken to establish a cadre of subject matter experts in the discipline of resilience. This cadre will be established during the year 2023/24. The theme for annual commander training in 2023/2024 will focus once again on recommendations from the Manchester Arena Inquiry, Airwave, National Occupational Standards (NOS), Minimal Occupational Standards (MOS) and Joint Organisation Learning (JOL).
Special Operations continue to coordinate with national colleagues from the National Ambulance Resilience Unit (NARU) courses for new commanders, and those undertaking refresher training.
Investing in the future of major incident response, the department has been integral in successfully submitting a business case for 16 new major incident vehicles to replace the current fleet. It had also been involved in the national procurement of two new mass casualty vehicles as well as receiving 2 new Polaris ATV along with purpose-built Polaris Carriers. Finally, work has been undertaken with national partners to develop the third iteration of the HART Fleet.
Other notable areas of work during the year included the ongoing support for the call for evidence for the Manchester Arena Inquiry following the publication of Volume Two:
Emergency Response, with 149 recommendations and 14 specific to our service, known as Monitored Recommendations. As we move forward to 2023/2024 and in preparation for the Covid-19 Public Inquiry preparatory work has also commenced.
Regional Operations Co-ordination Centre (ROCC)
The Regional Operations Co-ordination Centre (ROCC) is an integral part of the service and operates 24/7 365 days a year and provides an oversight across our emergency service areas. It also works closely with key stakeholders locally, regionally and nationally across the NHS, ambulance sector and other key partners such as police and the fire and rescue services.
The ROCC team incorporates oversight of demand and hospitals across the North West. This is done by the Regional Health Control Desk and the Greater Manchester Urgent and Emergency Care (UEC) Hub. This allows us to respond and invoke plans when needed during times of high demand or local challenges, enabling the organisation to flex its resources to respond to patients promptly.
Through the NHS industrial action, the ROCC have led Operation Constant Care, being the first touch point for senior leaders in the trust but also being a key stakeholder in joining many North West and national system calls, proving live situational briefs on ambulance performance, demand, hospital status and much more relevant to the system, and in particular patient flow.
Through our JESIP partners the ROCC has hosted many visits including senior officials from the Indonesian National Counter Terrorism Agency. This was a successful visit providing the international guests an insight into its role, with specific insight to its function in major and MTA incidents.
4.5 Patient Transport Services
Much of 2022/23 was influenced by the latter part of the Covid-19 pandemic and moving into a recovery phase from the pandemic. Although activity volumes were slow to recover in
the early part of the year, they quickly picked up pace from quarter 3 2022/23 when we were at approximately 85% of pre Covid-19 activity.
Overall activity during Month 12 (financial year) of 2022/23 was -8% (-10,954 journeys) below contract baseline whilst the cumulative position is -17% (-203,843 Journeys) below baseline.
Cumulatively, Cumbria is -30% below baseline, Greater Manchester is -5% below baseline, Lancashire is -30% below baseline and Merseyside is -7% below baseline.
| PTS ACTIVITY SUMMARY | |||||||||
Contract | Annual Baseline | Current Month Baseline | Current Month Activity | Current Month Activity Variance | Current Month Activity Variance% | Year to Date Baseline | Year to Date Activity | Year to Date Activity Variance | Year to Date Activity Variance% |
| Cumbria | 168,291 | 14,024 | 10,572 | (3,452) | (25%) | 126,218 | 87,843 | (38,375) | (30%) |
| GreaterManchester | 526,588 | 43,882 | 46,408 | 2,526 | 6% | 394,941 | 375,290 | (19,651) | (5%) |
| Lancashire | 589,180 | 49,098 | 38,438 | (10,660) | (22%) | 441,885 | 311,209 | (130,676) | (30%) |
| Merseyside | 300,123 | 25,010 | 25,643 | 633 | 3% | 225,092 | 209,951 | (15,141) | (7%) |
| NWAS | 1,584,182 | 132,015 | 121,061 | (10,954) | (8%) | 1,188,136 | 984,293 | (203,843) | (17%) |
Table 3: PTS cumulative activity variations as at Finance Month 12 – Contract Month 9 against contract baselines – Please note the 2022/23 PTS contract commenced 1st July 2022.
National Guidance regarding multi occupancy of PTS vehicles changed in April 2022 meaning that we could return to the pre Covid-19 position of transporting more than one patient on a vehicle, including taxis and volunteers. However, we decided to delay the implementation of this guidance until June 2022 to maintain patient and staff safety, particularly for our most vulnerable patients who are often immune-suppressed or frail.
During 2022, PTS continued to provide support to our emergency service with staff and vehicles. As Covid-19 regulations were lessened or withdrawn, and PTS work started to increase this support was reduced and by quarter 3 it was minimal, with many of the staff returning to PTS. We continued to support those staff that wanted to progress their career into PES and have enjoyed some success with our staff going into emergency medical technician, urgent care and apprenticeship roles.
Although these successes have been celebrated, this did put some resultant pressure on the service given the speed at which were able to recruit and our continued reliance on private ambulance resource to back fill vacancies.
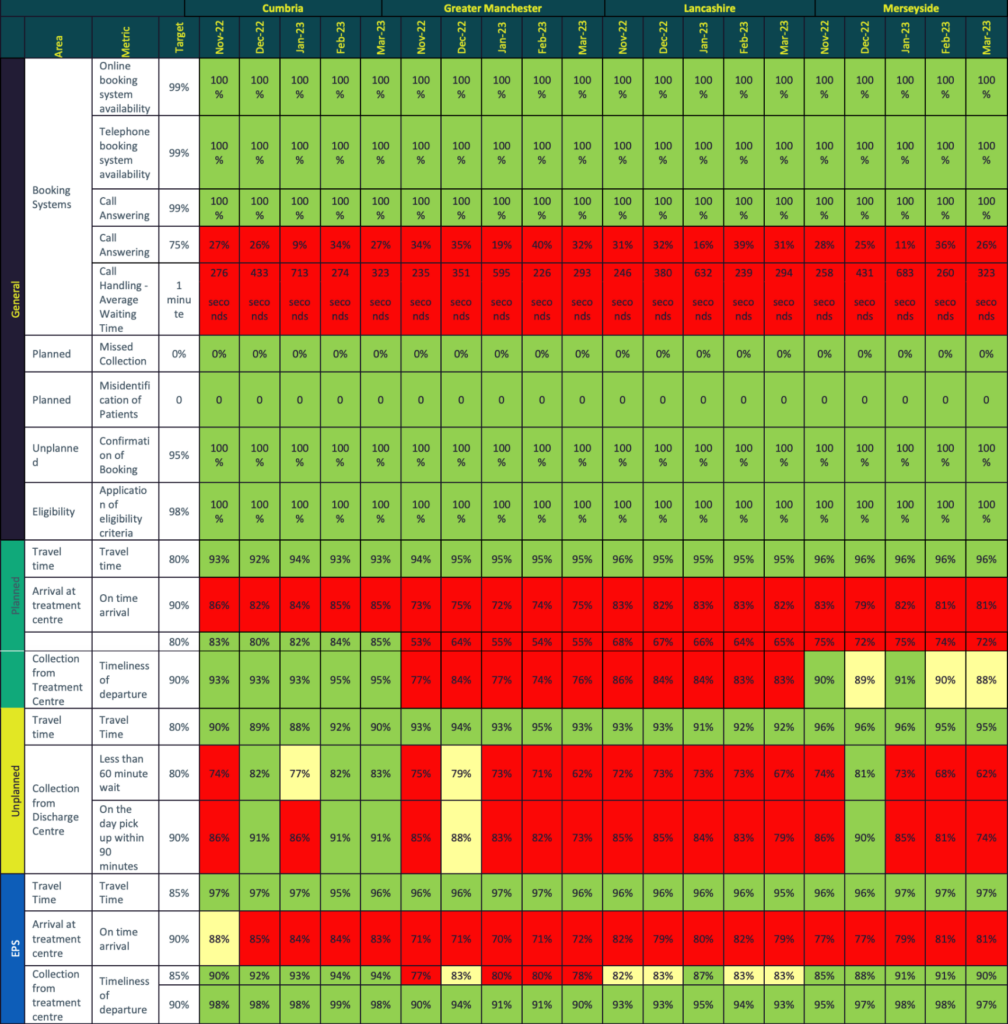
During winter 2022/23, PTS again provided a more responsive discharge service to support the improvement of flow in some of our busier hospitals and was able to discharge patients more quickly; in many cases within 60 minutes of the booked ready time. The key performance indicator for discharges is usually 80% in 60 minutes and 90% within 90 minutes. From 12 December 2022 to 05 February 2023 on average Monday to Friday 85% of discharges were collected within 60 minutes. Table 4 summarises the PTS performance against quality indicators.
During 2022/23 we began the recruitment of team leaders to achieve our objective of increasing our frontline supervision. Working with learning & development colleagues, an induction programme was developed to give this group of staff the best start in their roles as first line managers and this has been very well received. Although the recruitment is ongoing, PTS are in a much healthier position in terms of team leader numbers. Frontline supervision has increased from 24 in 2021/22 to 28 in April 2023 with 6 vacancies still to recruit to. These are currently covered by developing team leaders. We hope the team leader group will be fully established by September 2023.
Also, in the latter part of 2022/23 the PTS Bureau, which forms the Contact Centre and Control elements of PTS, successfully trained a small number of their staff in 999 calls and dispatch. Although this was primarily a response to the industrial action, it demonstrated that staff in PTS were enthusiastic and keen to provide the support and resilience and showed what is possible for the future.
Although activity volumes remained below baseline levels in some areas, PTS was able to utilise any resource capacity by taking an increased volume of low acuity activity that originated through the EOC for PES, again demonstrating collaborative and partnership working across service lines.
During 2022/23, private ambulance providers have continued to support the core PTS operation during its recovery from the seating capacity restrictions introduced because of
Covid-19. The support shown by our private ambulance provider partners has been critical in our ability to safely deliver services throughout the year. Further work has been ongoing in respect of providing assurance. This has taken the form of a contract specification review followed by inspections, to ensure the private ambulance providers meet our contractual requirements.
Volunteer car drivers are an integral part of providing a safe and effective patient transport operation and during 2022, recruitment recommenced and over 30 new volunteers joined the service. The “Star in a Car” campaign was relaunched to coincide with the recommencement of recruitment.
New child seats were purchased during 2022/23 and external training from an industry lead in the field of child seat safety was provided to all volunteers on how to safely secure a child in the seat.
During 2022/23 the following improvements were undertaken:
- System developments: A new version of the Cleric Patient Management System was introduced, and we continue to contribute to the development of this with the supplier.
- Text service: In March 2023 a new SMS text service was introduced to improve our service to patients. Those patients who opt in are notified via text to confirm their transport booking and can confirm or cancel transport by answering yes or no – freeing up valuable capacity. They are also notified by text when their transport is mobile and on the way to them. Analysis of the impact of this has not yet been undertaken as it is a new function.
- Transporting patients with dementia: As a result of learning from incidents, PTS changed the way in which we accepted booking requests and provided transport for patients with dementia; providing safer transport in a PTS Ambulance and not a taxi.
- Team Leader recruitment and induction: To improve visibility and engagement with staff, our front-line supervision group of team leaders was increased.
- Rapid Discharge Hub Winter: Faster more responsive discharge service to support flow with on average 85% of discharges between December 2022 and February 2023 collected within 60 minutes.
Going into 2023/24 the focus for PTS will be:
- To return to pre Covid-19 utilisation of, on average 1.8 patients transported per hour in an average 8-hour shift. During Covid-19 this dropped to 1.2 due to single occupancy of our vehicles. Currently, April 2023 utilisation is around 1.5.
- Better utilisation of taxis and volunteers will be an area of focus.
- The level of private ambulance usage has been reviewed and there is a plan to reduce this over time beginning in May 2023. This reduction will gather momentum as the year progresses subject to activity remaining stable and the PTS recruitment plan being achieved. The trajectory for this improvement is still in the planning stages and should be complete by the end of April 2024.
The priority will be to reduce spend in the third-party budget and balance that with an acceptable level of performance that maintains a safe service.
4.6 Community first responders
Community First Responders are volunteers who are trained and activated by us to attend a range of emergency calls, where a time critical response can make a difference to patient care and outcome. We have 567 active CFRs operating across all areas of the North West.
The responder provides care and support to the patient until the arrival of an emergency ambulance. Quite often, the role of a responder is one of reassurance and in some instances, for example when a patient has difficulty in breathing, simply giving oxygen can make a big difference. However, in extreme cases, the CFR can perform cardio-pulmonary resuscitation (CPR) or use a defibrillator to restart the heart. Chances of survival decrease by 10% with each minute that a person’s heart has stopped beating, and CFR availability in the local area can result in a quick response to ensure that treatment is started as early as possible, we currently have a bystander CPR rate of 83% and this treatment helps support the patient in the first minutes of an out of hospital cardiac arrest occurring.
We have continued to support, and proactively engage with communities, organisations, and individuals with the placement of Automated External Defibrillators (AEDs). These life saving devices are a vital part in increasing the chances of survival from a person suffering an out of hospital cardiac arrest. Within the North West we have over 6880 community public access defibrillators, which are devices that are available 24 hours a day, 7 days a week. These are placed in locked, heated, and coded boxes and members of the public can be directed to them in an emergency and instructed how to use via the emergency call taker in an emergency. In addition to these devices there are a further 6809 defibrillators registered with us that are in numerous buildings and again accessible if required. These buildings range from leisure centres, shopping centres, supermarkets, healthcare setting, schools etc.
We continue to work with the British Heart Foundation to embed the National Defibrillator Network know as ‘The Circuit’. This is a publicly accessible web-based system that allows direct registration of any accessible AED, and then it is directed to the appropriate ambulance service and allows for the emergency call takers to direct public to them in an emergency.
As we have emerged from the pandemic our CFRs have provided an estimated 132,296 hours of support both to our service and the communities of the North West. We have continued to provide support post incident for CFRs to ensure their wellbeing and their education is kept in line with the requirement of the NHS. All our volunteers are enrolled in statutory learning to ensure the care we deliver is of the highest standard.
In addition to this vital support many other tasks were supported by our volunteers, below outlines a snapshot of these:
- Crewed welfare vehicles: located at the numerous Emergency Department’s to allow crews access to refreshments. This provision meant operational staff were able to take much needed welfare breaks during the unprecedented winter period faced by the NHS. This was a new volunteer role within our trust and brought about a new way to allow volunteering for members of the public who did not want the traditional CFR elements. Since the vehicles were introduced, volunteers have given over 6485 hours of time to this role on 917 different duties. The feedback from both crews and volunteers has showed how the interaction benefitted all parties.
- Enhanced level of knowledge to responders; to allow them to attend lower acuity emergencies and have clinical support available to ascertain how best to support the patients’ needs and if an emergency ambulance was required for the patient. This has ensured we are able to prevent patients who may not of suffered an injury waiting a prolonged period and will for many gain access to local services in a timelier manner.
As we move forward, we are introducing a new digital way to mobilise CFRs across the region, bringing in new technology based on a smart phone application. This will enhance our communication capabilities between our responders and emergency operations centre, and benefit both patients and responder welfare.
Membership of a Community First Responder scheme is incredibly rewarding, and volunteers could be involved in saving someone’s life. Anyone who lives or works in the North West can get involved with their local CFR scheme, by either becoming a First
Responder or helping with other vital tasks such as fund-raising, support or administration.
Volunteers do not need previous first aid experience to join their local group, as full training will be provided. Further details on Community First Responder schemes are available at https://www.nwascfr.com.
5. Strategic aim: provide high quality and inclusive care
Section 5 to 7 of the Quality Account summarises what we have delivered during 2022/23 aligned to our strategic aim of providing high quality inclusive care that is safe, effective and person centred.
5. 1. Safety
Our goal is to develop the safest system for all patients and staff. This requires every staff member to understand their role and how they contribute to safety. Each year, our colleagues report more than 13,438 adverse incidents. The ambulance service is fraught with complexity and the risks of error have been well documented. Over the last decade, like most healthcare organisations, we have focused on improving governance, identifying risks, mitigating these through assurance processes and implementing learning. Safety has become core business and our strategy seeks to take these foundations to the next level focusing on safety improvement and strengthened safety culture.
During 2022/23 we invested in new roles to support patient safety including patient safety learning officers, senior patient safety learning manager and permanent funding for the strategic mental health team.
5.2 Effectiveness
Our goal is to provide clinically effective services using research evidence and agreed professional standards to improve clinical practice and service delivery through clinical audit, review, learning and improvement. In our Quality strategy, we focus on priority areas to improve the reliability of evidence-based care standards of:
- Cardiac arrest
- Stroke
- STEMI
- Sepsis
- Vulnerable patients (including frailty, mental health)
- Specialist services and preventing harm to patients who wait for our services (deterioration/self-harm)
Some of these conditions are measured nationally via ambulance clinical quality indicators. More details can be found in sections 7.4 and 7.4.1 of this document.
5.3 Patient Centred
Our goal is to listen to our patient feedback and use this to re-design personalised care. We interact with the North West population through several public engagement channels.
5.4 Pillars of Quality
Our fourth goal is to ensure that underlying processes of care, essential to delivering high quality care, are continuously improved. Importantly these ‘pillars of quality’ run through our organisation and there is no department or service line immune from ensuring that we deliver the highest standards of care under these domains. The six domains are:
- Complaints and Compliments
- Incident reporting and learning (including serious incidents)
- Safeguarding
- Health, safety, security, and fire
- Infection prevention and control (IPC)
- Medicines management
Our Quality strategy signals our intention to progress these six pillars of quality to previously unprecedented levels of performance.
6. Our improvement approach
6.1 Method
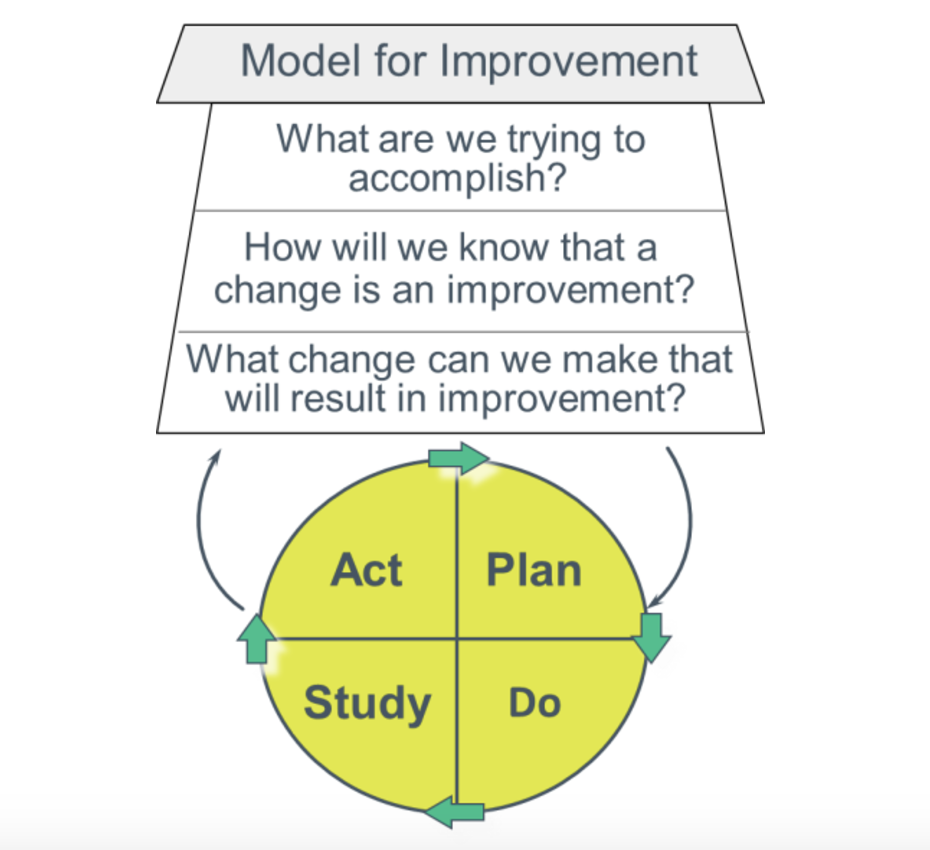
Our approach to improvement is grounded in the theoretical models of Deming, Juran and Shewhart. We use the Model for Improvement developed by the Institute for Healthcare Improvement. This is a method which asks teams to address three key questions and use Plan, Do, Study Act cycles to instigate small tests of change which build learning about how systems are working. This methodology is deceptively simple but has shown proven benefit across a range of industries. The Model for Improvement requires teams to focus on setting an explicit, measurable, time limited goal. It seeks agreement on a set of measures which will be tracked frequently (often daily or weekly) and asks teams to organise their thinking to focus on the specific changes which will make the most significant impact on the goals.
Organising these thoughts into a driver diagram or logic model helps teams to agree on leadership responsibilities.
6.2 Measurement and intelligence
We continue to commit to building a system of real time quality measurement and feedback to the service which can be used for performance, quality surveillance and improvement.
We are building measures for key programmes of work and providing real time data back to the service. During 2022/23 further developments have been made to Power BI reports which provide real time data through several self-access dashboards. Regular reports are shared from SafeCheck, our compliance platform, with quality and safety data triangulated in a quality compliance scorecard. The monthly integrated performance report provides assurance to the board each month on a range of indicators, including quality, effectiveness and patient experience.
6.3 Skills training
We continue to prioritise the building of improvement skills in individuals and teams, focusing on patient care priority areas. We continue to build our quality improvement network and design forums to systematically develop the talent and ideas of our workforce using techniques such as leadership development, patient stories, driver diagrams, process mapping, measurement of variation (statistical process control) and the Model for Improvement. Small tests of change, which build cyclically, are tested, and used throughout the organisation.
During 2022/23 Quality Improvement Network sessions have been delivered and the membership has increased to 201 members.
Topics covered at the 2022/23 Quality Improvement Network include:
- QI methods: Developing an aim statement, designing driver diagrams, creating PDSA cycles and process mapping.
- Theory: Spread and sustainability, culture and behavioural change and understanding the CQC assurance and compliance model.
- Engagement: Patient and public engagement methods and co design tools.
- Data: Measurement and collecting of data to understand the impact of improvements.
- QI and project documentation: How to apply data quality impact assessments to projects.
Case studies have included:
- Learning from the NHS England national rapid release policy pilot implemented at Royal Preston.
- Implementation of alternative transport to hospital project – Taxi in 5 roll out in Cheshire and Mersey.
- Public and Patient Panel members discussions about how to get people involved in work to shape delivery.
- Our compliance and assurance approach for third party ambulance providers.
- Internal quality assurance redesign project.
- Using quality improvement approaches to improve maternity care.
- Community First Responders (CFR) low acuity pilot using quality improvement approaches.
During 2022/23 staff have also been offered the opportunity to enrol on 90-minute QI virtual sessions covering the following topics:
- An introduction to quality improvement
- Starting your test of change
- Measurement for improvement
- Creating a change culture
Quality Improvement training delivery has continued virtually to make it more accessible for shift working, organisational geographic spread and new ways of working since the pandemic.
Our Digital Design Forum has continued to provide a space for staff to bring ideas or issues and work with our digital team to use improvement methods to test digital solutions.
6.4 Quality assurance visits
We continue to focus on the design and testing of a standardised process for internal quality assurance. Importantly the quality visits reward those teams who perform well with an acknowledged performance status and identify those areas requiring further support and more frequent review. The implementation of this system of visits is critical to ensuring management oversight and corporate assurance on key standards.
6.5 Evaluation
In its second year as a department, the evaluation function has enjoyed continued growth. The primary evaluation from 2021/22, Emergency Department contract cleaning has been distributed internally with aspirations to publish externally in 2023. The ongoing large-scale work is a trust-wide evaluation of video consultations due for internal release in summer 2023 and external release later this year. In 2022/23 the evaluation team have supported pilots and rollout of digital innovations including SMART site pilot (Kendal Station), Aspirer digital timesheets, SafeCheck vehicle checks, and asset tracking. The growth of the department has allowed the team to increase its footprint, providing support to:
- Quality Improvement’s handover collaborative with a Blackburn emergency department case study.
- Strategy, Planning and Transformation’s internal evaluation of our strategy.
- Evaluating our digital capability.
The Evaluation team aims to raise its profile further in 2023/24, with the planned publication of the Evaluation Plan and SharePoint site. This will be directed by collaboration initiatives, in which the team will work alongside colleagues from operations and corporate
services to ensure developments have appropriate evaluation support, be it from within the department or by providing support to colleagues.
7. Our improvements 2022/23
7.1 Safety
Patient safety partners
We have recruited three Patient Safety Partners from our Patient and Public Panel, with a range of experiences and knowledge to partner with us to contribute to our management of patient safety within North West Ambulance Service. Recruitment took place in collaboration with our patient engagement manager working with the panel. All panel members were offered the opportunity to express an interest in the role of Patient Safety Partner. All panel members who expressed an interest were recruited to phase 1 following the recruitment process, with ongoing support to ensure that all panel members can fulfil the role and any additional requirements or development needs are supported. In phase 2 of recruitment, we plan to expand recruitment beyond the patient and public panel to ensure our cohort of patient safety partners can collaborate with us on a wide range of patient safety improvements and ensure a wide range and diversity of views and lived experiences. Our Patient Safety Partners have undergone induction, and will be embedded in the following areas of work during 2023/24:
- Membership of safety related committees, sub-committees, and groups to include analysis and review of safety related data.
- Involvement in patient safety related improvement projects.
- Working with our organisation, and our service users to consider how we might improve safety within the organisation.
- Participate in patient safety related training and learning for our people.
- Work closely with our Patient Safety teams to embed Patient Safety Incident Response Framework.
Patient stories
Duty of Candour is a statutory requirement for NHS organisations, and the principle of being open and transparent with patients is an essential element of the care we deliver to our service users. In 2022/23, North West Ambulance Service has undertaken significant work to enhance Duty of Candour, and the experience of patients where harm has occurred including:
To help us learn from when things go right, and when things go wrong, we continue to develop a suite of patient stories, told by patients or significant others through their eyes, about their lived experience. These stories are shared with our staff through groups, sub- committees and Committees and have been utilised to prompt discussion and subsequent action on a variety of topics. These stories are also used to support data during our improvement work across the system, such as working with our partners in the acute trusts to reduce delays in handover of care at emergency departments.
Duty of Candour
- Use of technology to strengthen our ability to highlight harm at the earliest opportunity and respond in a timely manner to apologise and learn from events.
- A refreshed and updated Duty of Candour procedure.
- Design and delivery of bespoke Duty of Candour training across the organisation.
- Involvement of patients and families who have experienced harm in our organisational learning through patient stories.
Safety governance
The safety of our patients and staff has continued to be a priority for us in 2022/23 and assurance of our ongoing commitment to continuous safety improvement, is overseen through governance structure including the Health, Safety, Security and Fire sub-committee, Patient Safety sub-committee and Clinical Effectiveness sub-committee. Each subcommittee provides a chairs assurance report to the Quality and Performance committee that we are delivering the required standards and improvement, and reporting any risks identified.
These also feed into our commissioner regional meetings with representation from each ICB
for the Quality and Safety Group to give further assurance on safety. In 2022/23 each sub- committee has been assessed against its terms of reference to understand what governance changes were required to meet the delivery of work programmes.
Safety culture
In 2022/23 work has been undertaken to improve safety culture in the organisation. Building upon the results of the NHS staff survey, we have commenced and will scale up in 2023/24, safety culture surveys and qualitative conversations using the Manchester Patient Safety Framework to explore the detail of the information we received. Each area and sector will have their own bespoke improvement plan to improve safety culture within teams. Work has also continued to ensure that staff reporting incidents/events are able to receive appropriate feedback with the launch of Datix Cloud IQ platform, with plans for increased focus on learning from excellence, as well as where things do not right.
Just Culture principles continue to be embedded across the organisation, with further work planned to take place in 2023/24 as part of the launch of the new Patient Safety Incident Response Framework in the autumn of 2023.
Safety learning
The organisation has in place policies and procedures which set out how we learn from incidents and events including:
- Learning framework
- Learning from experiences policy
Each area also has an established learning forum, and a debrief process in place to share learning that is generated from a range of insights such as incidents, serious incidents, claims, inquests and safeguarding. There are several additional ways that learning is disseminated including clinical and non-clinical bulletins and online and face to face learning. We also have in place governance systems to oversee themes of learning and gain assurance that we have continuous improvement because of the identification of learning.
During 2022/23 we have seen significant improvement taking place because of safety learning such as:
- Introduction of NHS Pathways
- Developments around maternity and mental health
- Collaboratives relating to hospital handover
- Digital innovation
We also have robust processes in place to work with external organisations such as the Healthcare Safety Investigations Branch (HSIB) to ensure that we learn proactively, and as a result of any independent recommendations.
Whilst a vast amount of work has taken place in 2022/23, we are also preparing for further opportunities in 2023/24 to enhance how we learn with a range of additional tools that we will introduce as part of our launch of Patient Safety Incident Response Framework (PSIRF) and the introduction of a new Patient Safety Learning team.
Safety skills
With ongoing system pressures, some elements of safety skills training have been paused, however despite the pressures experienced we have continued to make progress, with initial roll out of Level 1 and 2 of the Patient Safety Syllabus, with a plan to scale up in 2023/24. This incorporates:
- Systems approach to patient safety
- Learning from incidents
- Human factors, human performance, and safety management
- Creating safe systems
- Being sure about safety
Members of our leadership team and Patient Safety team have also completed Patient Safety Incident Response Framework Training (PSIRF), and the Health Care Investigations Branch Investigations Training ( Level 3) to gain a greater understanding of using a systems approach to investigations, which will replace the root cause analysis methodology with the launch of PSIRF, and strengthen our knowledge and understanding of human factors and
using differing approaches to learning in the organisation. There has also been bespoke skills training in response to incidents across the organisation, for example delivery of bespoke obstetric emergency training from our maternity team.
Patient Safety Incident Response Framework
During autumn of 2023, NHS organisations will transition from the Serious Incident Framework (SIF) to Patient Safety Incident Response Framework (PSIRF) which is a fundamental change to the way to the way we manage and respond to Patient Safety Incidents for the purpose of learning and improving patient safety. During 2022/23, there has been significant work to prepare for this transition which has involved:
- The recruitment of an implementation lead, who will focus on embedding the framework in our service.
- Communications with internal and external stakeholders.
- Engagement with organisations that have already piloted PSIRF.
- Transition and development of our incident reporting platform.
- Recruitment of Patient Safety Partners.
- Duty of Candour review and improvement work.
- Safety culture review and improvement work.
- Bespoke PSIRF training for staff.
- Review of our learning systems and processes.
Safety insights
We have developed our ability to not only use data from a range of insights such as incidents, serious incidents, complaints, compliments and claims, and learn from this. We have also developed a range of dashboards that allow us to monitor and respond to data in real time. Over the winter, we used this data to undertake a detailed review of incidents that resulted in patient harm and shared this with partners across the healthcare system to inform planning for the coming year. In addition to data insights, we are also passionate about understanding what our patients have to tell us about their care, and regularly use patient stories to inform our learning.
Clinical Safety Plan
The Patient Safety Plan has been reviewed and renamed “Clinical Safety Plan”. The revised version offers more sensitive and specific measure for surges in demand and interventions to address the specific causes of surge. It includes the altering of call handling scripts to encourage self-conveyance, automated messages for referring health care professionals and SMS messaging for callers. The Clinical Safety Plan dashboard offers a more holistic overview of potential risks to patient safety, and it provides an overall escalation level based on a risk stratification of multiple metrics.
Also, included within the Clinical Safety Plan are a suite of interventions, including the Clinical Response in surge. This builds on lessons learnt through circuit breakers, critical incidents and industrial action to allow for increased clinical focus on waiting patients, ensuring effective and efficient use of our resource. This methodology has been shown to increase our hear and treat rates significantly during periods of surge and allows for continual clinical review of high-risk patients.
7.2 Speaking up
We are committed to an open and honest culture, maintaining high standards of patient care, continuously striving to act honesty and with integrity in our approach to the management of systems, processes, responsibility as an employer and protecting the people within the communities that we serve from harm.
Freedom to Speak Up (FTSU) activity 2022/23
During 2022/23 the Freedom to Speak Up Guardians saw a 3% increase in cases on the previous reporting period with 100 concerns being raised via the Guardians. The themes are similar to the previous reporting period with concerns revolving around human resource matters, an increasing number of patient safety concerns and sadly an increase in concerns connected to racism and sexist behaviours. The chart shows the breakdown of themes as required by the National Guardians Office (NGO) and the number of concerns by theme per service line.
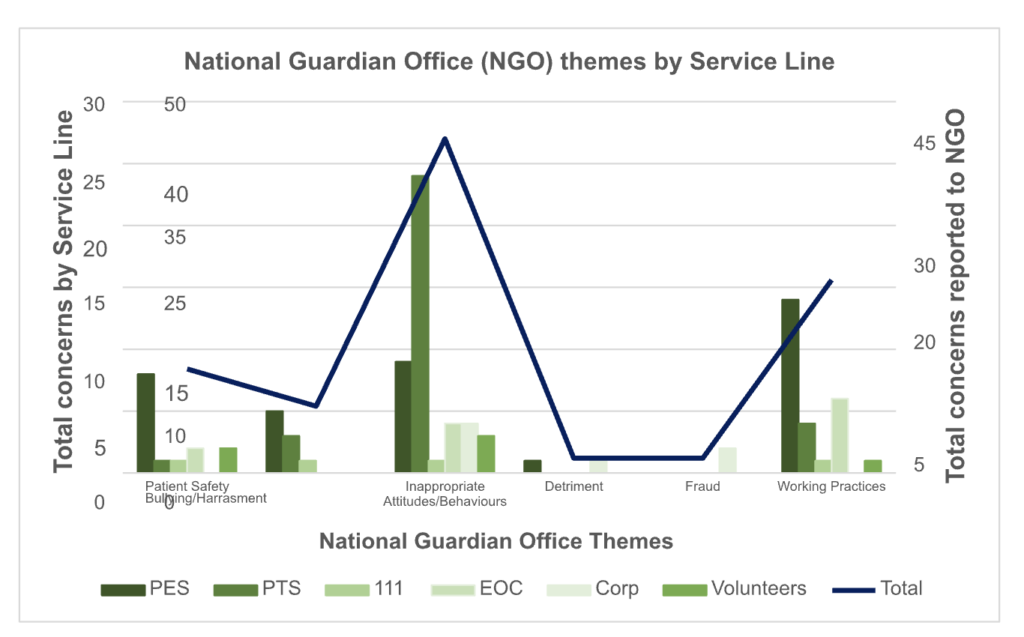
2022/23 has been a busy year for the Freedom to Speak Up Guardians, below is a summary of what has happened during 2022/23:
- Guardian recruitment: we employed two part time Guardians. Both Guardians held FTSU as an additional role and the team was expanded further employing administration support and an additional full time Guardian in June 2022.
- Refresh: Freedom to Speak Up underwent a refresh, with new posters and banners created. The internal Green Room page had a refresh and introduced a new anonymous tool to raise a concern.
- Freedom to Speak Up Policy: A new national Freedom to Speak Up policy was published by NHS England and trusts had to utilise this policy as a base for their own. A new simpler and streamlined policy was introduced in January 2023, which makes it easier for our people to raise concerns.
- Ways to Speak Up: Following the introduction of the new policy, new ways to Speak Up were introduced. Alongside the existing routes of email, phone and letter, the Guardian team have utilised our digital offer and developed an online form, WhatsApp and Twitter.
- Freedom to Speak Up month: October 2022 saw the national Freedom to Speak Up month. With support from our communications team, a detailed plan was created. This consisted of bulletin pieces, videos explaining FTSU and a roadshow which included five days of travelling around the region’s emergency departments. In addition, there were engagement events with Patient Transport Service and volunteers, a visible presence in EOC’s and corporate sites and an increased number of operational shifts. This was also a good opportunity to work with the Race Equality Chair, not only during Freedom to Speak Up month but also Black History Month.
- Education and learning: A change in the national requirements for e-learning meant a change to our online offer. We have allocated time for the mandated ‘Speak Up’ module for all staff and the ‘Listen Up’ module for managers. This year we have mandated the ‘Follow Up’ module for all senior leaders. The Freedom to Speak Up team have also engaged with the education and training team and have attended several new employee inductions sessions alongside linking in with all the universities we work with to talk about the importance of speaking up.
- Staff forums: The Guardians have attended several staff forums.
- National Freedom to Speak Up Guardian conference: we were represented at the National FTSU Guardian conference in London. This was an opportunity to hear from the CQC and others as to the changes being made to closer review speaking up arrangements in NHS trusts.
- CEO meetings: We continue to be supported by our Chief Executive, Medical Director and Director of People with a monthly meeting to discuss FTSU themes and concerns.
- Non-Exec Director meetings: We also continue to be supported by our Non- Executive Director with a monthly meeting to offer assurance of our speaking up arrangements and an opportunity to discuss any concerns.
- Reports: 2022/23 saw several reports published with a focus on speaking up, cultural concerns and patient safety. In February, the National Guardians Office released their report into speaking up with English ambulance trusts. Following this, the FTSU Guardian team completed a gap analysis based on the recommendations and will now look, alongside other directorates to implement the recommendations. CQC
reports from other organisations have allowed for further learning and changes to our own systems.
It is hoped that the changes made to FTSU in the last 12 months will have created a solid foundation on which we can further build our speak up culture, ensuring we embed listening up, a culture of problem sensing and inquisitiveness. Only by doing this will we ensure we listen to every voice and in turn save careers, relationships and lives.
7.3 Learning from Deaths
Our approach to learning from deaths goes far beyond a process of simply counting, classifying and reporting deaths, it is a commitment to supporting our journey towards providing an outstanding service to patients, their families and carers. We can protect future patients from avoidable harm, reduce unwarranted variation and provide truly patient centred care.
Our approach to Learning from Deaths goes far beyond a process of simply counting, classifying and reporting deaths; it is a commitment to supporting our journey towards providing an outstanding service to patients, their families and carers. We can protect future patients from avoidable harm, reduce unwarranted variation and provide truly patient centred care.
In the past year we have met all reporting requirements with quarterly Learning from Deaths reports being received and reviewed through our corporate governance structure and ultimately by our Board for approval. The table below details the number of deaths reviewed and the number of deaths where problems in care have contributed.
| 2022/23 Learning from deaths | Total Number of Deaths in scope | Total number of Deaths Reviewed | % Deaths Reviewed | Total number of deaths where problems in care have contributed |
| Q1 | 94 | 83 | 86.3% | 17 |
| Q2 | 144 | 124 | 86.1% | 12 |
| Q3 | 168 | 80 | 47.6% | 25 |
| Q4 | Currently in progress | Currently in progress | Currently in progress | Currently in progress |
| Year-to-date | 406 | 287 | 70.7% | 54 |
The main contributory factors to patient deaths were attributed to problems in EOC procedures, specifically calls being incorrectly categorised and lack of available resources to allocate to incidents. The structured judgement review (SJR) process identified most patients received appropriate care, but where failings occurred these included the failure to record observations, assessment, investigations, capacity to consent not assessed correctly, triage tools used inappropriately and poor clinical documentation.
The SJR process has identified areas of good practice such as holistic decisions not to resuscitate, recognition of end-of-life care and challenged health care professionals plan when no end-of-life care plan exists, patient centre decisions, and coordinated care with GP and families.
During 2022/23 we have improved and delivered our Learning from Deaths (LfD) programme by:
- Meeting national reporting requirements.
- Engaging with our Patient Public and Panel (PPP) representatives at moderation panels.
- Involving Emergency Operations Centre Specialists in structured judgement reviews (SJR). This change means we are fully compliant with the LfD framework. Our first panel with EOC specialists met in March 2023 and there have been some immediate learning for EOC processes.
- A commitment to disseminate and promote good practice has been made by the Consultant Paramedic through the area learning forums and individual frontline staff.
7.4 Effectiveness
Our goal is to provide high quality inclusive care using research evidence and agreed professional standards to improve clinical practice and service delivery through clinical audit, review, learning and improvement. The national Ambulance Clinical Quality Indicators focus on priority areas to improve the reliability of evidence-based care standards of:
- Cardiac arrest
- Stroke
- STEMI
- Sepsis (Retired measure from September 2022)
- Falls (New measure from June 2023)
We have worked with national stakeholders to drive the development of the new national falls indicator and are modelling currently how we can measure and improve the care we provide patients who fall and require our services.
We have fully adopted all nationally recommended changes to clinical practice guidelines through the Joint Royal College Ambulance Liaison Committee (JRCALC) and our staff have the most up to date versions of guidelines available digitally at their fingertips.
Our clinical audit focus for 2023/24 will be the development of localised performance data for our clinicians and to use that data to drive quality improvements for patient outcome and care bundle compliance.
Other falls work we are involved in includes national directives where we have worked with internal and external stakeholders and ICB partners to review and enhance the provision available for patients who fall. This is being delivered through community responses to patients who require lifting off the floor and we continue to monitor utilisation of these services through our Clinical Hub.
7.4.1 The Ambulance Clinical Quality Indicators (ACQIs)
Our key measure of the effectiveness of our services is the National ACQI submission to NHS England. This is produced each month by the Clinical Audit team and used by clinical leadership to inform their local improvement and feedback to staff.
There are clinical leads for each of the indicators who lead working groups and work with system partners to learn and share outcomes. Local reporting on the National ACQIs is received quarterly at our Quality and Performance Committee and the Clinical Effectiveness sub-committee. Further localised reporting is provided to the clinical leads for cardiac arrest, STEMI, stroke and sepsis to contribute to learning and improvement in the quality of healthcare provided. We submit our ACQI outcomes and performance monthly as part of the national NHS England return and these are reviewed at joint meetings with our commissioners at the Clinical Quality Assurance Committee.
Data collection for these indicators occurs three months in arrears, so the performance data displayed in the below tables are for quarter one to quarter three 2022/23. To note the Sepsis ACQI has been retired and an Older Adult Falls ACQI will be piloted using March 2023 data.
| National Ambulance Clinical Quality Indicator | November Performance2021/2022 | November Performance2022/23 | NovemberNational Average 2022/23 |
| Cardiac Arrest (All –ROSC at Hospital) | 28.5%(92/323) | 29.3%(105/358) | 27.8%(827/2978) |
| Cardiac Arrest (Utstein – ROSC at Hospital) | 52.8%(28/53) | 34.7%(17/49) | 48.2%(214/444) |
| Cardiac Arrest (All –Survival to 30 days) | 8.0%(25/314) | 4.2%(15/356) | 7.8%(229/2935) |
| Cardiac Arrest (Utstein – Survival to 30 days) | 22.4%(11/49) | 16.3%(8/49) | 25.1%(106/423) |
| STEMI PPCI Patients (Call to Angiography) | 03:00:00(109) | 02:41:00(131) | 02:30:00(899) |
| Confirmed Stroke Patients (Call to Door) | 01:51:00(522) | 01:41:00(516) | 01:47:00(4334) |
| Diagnostic Stroke Care Bundle | 97.4%(856/879) | 97.4%(1048/1076) | 97.2%(8765/9022) |
Data Source: NHS England. 2022. Ambulance Quality Indicators 2022/23. [ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality- indicators/ambulance-quality-indicators-data-2022-23/ [Accessed 13 April 2023].
Stroke Care Bundle
| Reporting Period: April 2022 –November 2022 | AQI Care Bundle Performance | NWAS: Outcomes from Stroke Care Bundle | National Average & Range |
| April 2022 | No National Data Published | ||
| May 2022 | 97.1% | 96.4% | |
| June 2022 | No National Data Published | ||
| July 2022 | No National Data Published | ||
| August 2022 | 96.3% | 95.9% | |
| September 2022 | No National Data Published | ||
| October 2022 | No National Data Published | ||
| November 2022 | 97.4% | 97.2% | |
| December 2022 | National data not published at the time of writing | ||
| January 2023 | |||
| February 2023 | |||
| March 2023 | |||
ACQI Stroke Diagnostic Bundle data. Data Source: NHS England. 2022. Ambulance Quality Indicators 2022/23. [ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical- work-areas/ambulance-quality-indicators/ambulance-quality-indicators-data-2022-23/ [Accessed 13 April 2023].
Acute ST-elevation Myocardial Infarction Care (STEMI) Bundle
| Reporting Period: April 2022 –November 2022 | AQI Care Bundle Performance | NWAS: Outcomes from STEMI Care Bundle | National Average & Range |
| April 2022 | 64.2% | 72.0% | |
| May 2022 | No National Data Published | ||
| June 2022 | No National Data Published | ||
| July 2022 | 67.9% | 73.6% | |
| August 2022 | No National Data Published | ||
| September 2022 | No National Data Published | ||
| October 2022 | 68.5% | 72.7% | |
| November 2022 | No National Data Published | ||
| December 2022 | No National Data Published | ||
| January 2023 | National data not published at the time of writing | ||
Data Source: NHS England. 2022. Ambulance Quality Indicators 2022/23. [ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance- quality-indicators/ambulance-quality-indicators-data-2022-23/ [Accessed 13 April 2023].
Post ROSC Care Bundle
| Reporting Period: April 2022 –November 2022 | AQI Care Bundle Performance | NWAS: Outcomes from Cardiac Care Bundle | National Average & Range |
| April 2022 | 76.5% | 78.6% | |
| May 2022 | No National Data Published | ||
| June 2022 | No National Data Published | ||
| July 2022 | 70.2% | 77.0% | |
| August 2022 | No National Data Published | ||
| September 2022 | No National Data Published | ||
| October 2022 | 73.8% | 76.5% | |
| November 2022 | No National Data Published | ||
| December 2022 | No National Data Published | ||
| January 2023 | National data not published at the time of writing | ||
Data Source: NHS England. 2022. Ambulance Quality Indicators 2022/23. [ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality- indicators/ambulance-quality-indicators-data-2022-23/ [Accessed 13 April 2023].
Sepsis Care Bundle
| Reporting Period: April 2022 – June 2022 | AQI Care Bundle Performance | NWAS: Outcomes from Sepsis Care Bundle | National Average & Range |
| April 2022 | No National Data Published | ||
| May 2022 | No National Data Published | ||
| June 2022 | 67.3% | 83.9% | |
| July 2022 | No National Data Published | ||
| August 2022 | No National Data Published | ||
| September 2022 | ACQI retired and will be replaced with Older Adult Falls – March 2023 data | ||
| October 2022 | |||
| November 2022 | |||
| December 2022 | |||
| January 2023 | |||
| February 2023 | |||
| March 2023 | |||
Table 10: ACQI Sepsis care bundle data
Data Source: NHS England. 2022. Ambulance Quality Indicators 2022/23. [ONLINE] Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality- indicators/ambulance-quality-indicators-data-2022-23/ [Accessed 13 April 2023].
Clinical audit
We successfully transitioned from a paper-based paramedic emergency service patient record to an electronic patient record (EPR). The electronic record supports clinicians in offering condition specific sections with pre-determined data entry (where appropriate) in addition to ‘free type space’ for more detailed data entry.
The move to an EPR has required the development of an in-house clinical audit tool called Apex. The development group is a multi-disciplinary team and includes digital developers and specialists in the use of Power Business Intelligence (BI) systems working closely with the clinical audit team. The team has successfully completed three of the five required modules for national mandatory clinical audit. It has been possible to realise some of the anticipated benefits in terms of reducing the number of systems the auditors have historically had to access to complete the audit. Apex remains in phase one development – and the scope is to deliver an audit mechanism for each of the AQIs, with an output suitable for several audiences including the national submission requirements, and frontline staff members as a personal clinical development indicator. Phase one is close to completion with Apex modules for stroke, Sepsis and STEMI AQIs available for audit use.
Priorities for 2023/24 are to scope and progress Apex phase 2 to deliver granular clinical audit data which can be used to develop clinically led local improvement plans.
7.4.2 Reducing handover delays
Hospital handover delays have continued to be a challenge for us and worsened during 2022/23. This picture has been reflected by other ambulance services across the UK. We have been working in partnership with emergency department teams, hospital senior management teams and with commissioners to address the handover challenges from a system perspective.
Figure 8 below summarises our average turnaround time from April 2019 to March 2023.
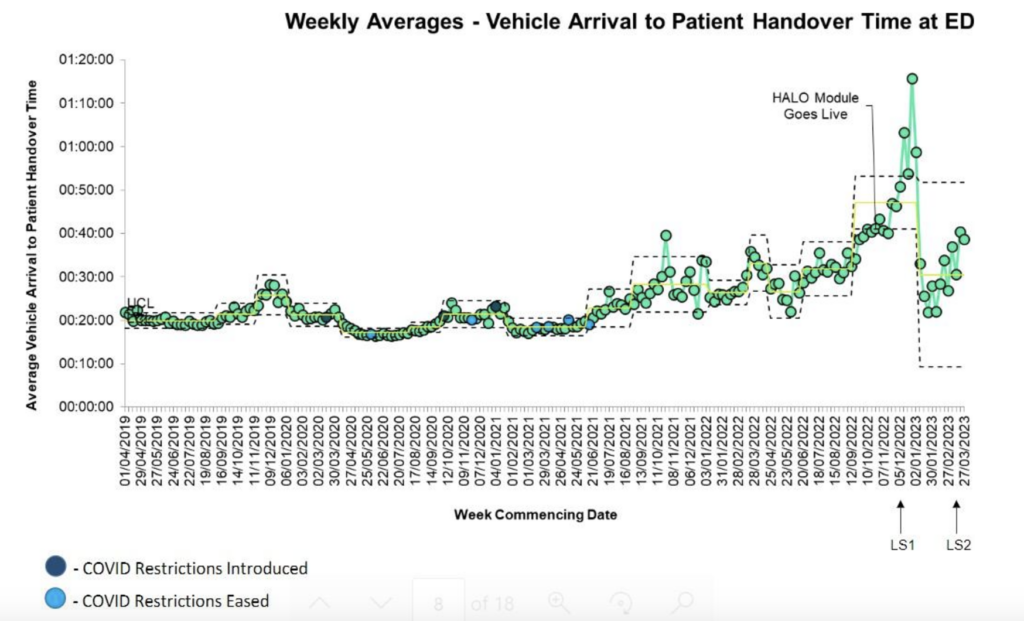
Figure 8: Handover times run chart 2019-2023
We have been leading quality improvement programmes around hospital handover since 2018. During October 2022 a Regional Handover Board was established to lead a North West Hospital Handover Collaborative across the three Integrated Care Board (ICB) footprints of Cheshire and Mersey, Greater Manchester and Lancashire and South Cumbria (including North Cumbria). The Board consists of representation from our service, NHS England, ICB leads, hospital Chief Executive leads who have acted as Executive Senior Responsible Officers (SRO) and Advancing Quality Alliance (Aqua). NHS England have sponsored this work and commissioned Aqua to deliver the collaborative learning sessions with us. Chief Executive SRO leads and ICB leads agreed to lead handover collaboratives across their local systems. GM have set up fortnightly meetings for this work. Lancashire and Cumbria teams have aligned their work to internal quality improvement programmes.
NHS England and Aqua are partners in delivering the handover collaborative and the North West handover improvement programme was launched in December 2022. Over 250 people from 32 organisations attended the learning sessions. There was representation from our service, emergency departments, community, commissioning, mental health teams and public and patients’ involvement via the Patient and Public Panel and
Healthwatch. The stretch aim for the collaborative was to reduce 60-minute handovers by 50% by March 23. All sites signed up to this aim and some set more ambitious aims for their local areas. Most of the North West hospitals had a rep at one of the events.
Further events were planned for early February 2023 but had to be rearranged to March and April 2023 due to date clashes with NHS industrial action dates. Real system engagement has been evident at the learning events. A final session was organised for the 23 May 2023 which brought all teams from the North West together. At the event it was revealed cumulatively the collaborative achieved a 47% reduction in 60-minute handover delays, with many hospitals achieving far more despite winter pressures.
Key work that has been undertaken during 2022/23 includes:
- Continued local sector involvement with the 3 acute sites who are part of the national NHS England hospital handover programme. These are Royal Oldham, Whiston and Morecambe Bay hospitals (Royal Lancaster and Furness General).
- Development of a Future NHS platform to support the delivery of the hospital handover collaborative.
- Sharing hospital monthly data packs with all North West hospitals and commissioning leads to identify areas for handover improvement or to identify areas where improvements have occurred.
- On site quality improvement coaching at hospitals with local teams to support the implementation of the ambulance handover safety checklist and escalation cards.
- Executive to executive conversations which focus on improving patient safety, addressing handover challenges, and sharing ideas for improvement.
- Implementation of the HALO module on the hospital arrival screen.
- Focused quality improvement work at the Regional Operations Control Centre.
- Engagement at local, regional, and national forums sharing the work undertaken by us to improve handover. This work was a Health Service Journal 2022 finalist in the patient safety category.
- Public health
We are taking a proactive approach to public health, working with communities and partner organisations to identify and deliver preventative initiatives to improve the health of the North West population. Our aim is to contribute to improving physical and mental health and reducing health inequalities.
We were the first ambulance service in the country to host public health registrars. In 2021, we established our first Population Health Delivery Group to support delivery of public health initiatives in the organisation. Our 2022/23 Public Health Plan identified the following opportunities to develop:
Strategy
- We contributed to the trust strategy and supporting sub-strategies. Our aim has been to ensure prevention and reduction of health inequalities are considered as integral part of our work. We have also contributed to the development of a national position statement reaching a consensus about the ambulance sector’s role in tackling health inequalities.
- Working with our Partnership Integration Managers, we have supported ICBs across our footprint, identifying ways to add value to their prevention and inequalities work. In this area, we have developed analysis on high frequency locations, which we have shared with ICS partners in Greater Manchester and Cumbria and Lancashire to support system urgent care demand prevention work.
- We have had an overarching role in coordinating, monitoring and evaluating social value work, helping to bring outputs together in one place. To champion our role in this area, we signed up to the Cheshire and Merseyside Population Health Board’s
Prevention pledge, which builds on the social value award we received from the region in 2022.
Data and intelligence
- We are identifying opportunities to develop the use of our data to improve a targeted and preventative focus across the wider ICSs we operate within.
- As part of this work, we undertook an initial analysis of 111 activity, highlighting areas of exceptional demand and are working with ICSs to understand reasons for the differences observed. We have also initiated work to analyse and establish a baseline for equity of access in PTS. Externally, we are paving the way for wide scale sharing of blood pressure data to support hypertension case finding in primary care.
Building capability
- Our vision is for our employees is to be equipped with the skills, knowledge and attributes at three levels of competency: fundamental knowledge and skills such as confidence in behaviour change conversations for the front-line; advanced skills and support to lead quality improvement projects for those with more interest or experience and relevant roles; and specialist public health leadership capacity including analytics.
- Although some public health training is included in undergraduate training for paramedics, there is no in-house mandatory training specific to public health. We have identified resources with Health Education England, Public Health England, Office for Health Improvement and Disparities. Our Public Health Delivery Group input has suggested we develop a shared language and interest in Public Health across our service ahead of us facilitating access to these training resources. In the meantime, we are sharing fundamental public health knowledge and supporting those with an interest to lead public health projects. As part of this, we delivered a Paramedic and Public Health module on the Paramedic master’s course at Liverpool John Moores.
Supporting delivery
- Our vision is to have new commissioning arrangements in place which support us in delivering public health initiatives. As a first step we are developing capacity to identify and influence external funding opportunities. In addition to the Public Health Delivery group, we have hosted four Public Health Registrars, we have recruited a permanent Public Health Manager post, and we are exploring recruitment of a Public Health Consultant post to offer senior leadership and expertise and support our establishment as a sustainable placement for Public Health Registrars.
- To support implementation, we have established a Social Prescribing Working group to map and promote social prescribing pathways across our blue light services. We have conducted significant work on information governance, establishing over 20 pathways and their digital integration. To support implementation, we have developed communications, a webpage and are building on this using a Health Education England grant to develop training materials for PTS crews to support make every contact count, including referral to social prescribing services.
- Specialist services and preventing harm to patients who wait for our services
Maternity care
We currently provide both telephone and face to face maternity care by a range of ambulance staff including paramedics, and non-registered ambulance staff, with the capability to include the NHS 111 service within its portfolio. Maternity patients and newborns remain a key patient priority group for us, highlighting the need for a clear approach to addressing current improvement and quality efforts relating to prehospital maternity and newborn care. Reducing unwarranted variation in experience or outcome is a focus for us. During 2022/23 we appointed a substantive Consultant Midwife to support implementation of the recommendation of the 2022 NWAS maternity report, including a self-assessment against the national Ockenden report. The release of the single maternity
plan in 2023 is a pivotal moment for the national maternity transformation plan. An amalgamation of the Ockenden review and the East Kent report, an implementation plan aligned to immediate and essential actions detailed in national safety reports, provides healthcare systems with the national plan to enhance safe and personalised maternity and newborn care.
The focus for this area of work during 2022/23 has been:
- Incident reporting: The NWAS maternity dashboard, coupled with safety incident reporting analysis has supported focus for improvement. Following a triangulation of data, recommendations for focus have influenced and informed key training objectives for the maternity team. In addition, learning from incidents included in wider senior clinical learning forums across the service and externally following joint case reviews.
- Patient safety: Guided by the NHS Single Maternity plan we will work in collaboration with the regional maternity team to support local and regional actions to support safe and effective maternity and newborn care, to ensure these patients receive the right care and the right time in the right place. During 2022/23 we have led on number of national initiatives to support focus on pre-hospital maternity and newborn care, including the appointment of one of our advanced paramedics as chair of the maternity national ambulance leads group.
- Training and education: Following on from 2021/22 summary, our pre-hospital PROMPT pilot was the first evaluation undertaken in the UK within an ambulance service.
Evaluation results identify the impact on clinicians’ skills and confidence in managing maternity and newborn incidents. 2023/24 focus is to explore the sustainability and implementation of this model of training across our service and to explore multi- disciplinary team approaches to training with and across maternity teams.
- System working and collaboration: Supporting system working the Consultant Midwife has built key relationships with the local maternity systems (LMS) across the region, reporting into each of the LMS boards and the North West regional perinatal board. Timely multi-disciplinary team approach to local and regional challenges has identified collaborative opportunities for joint training and shared learning form incidents, where
applicable. Regional relationships have supported the timely review of policies and pathways into care, supporting a patient focused approach to system working, reducing regional variations in care. Exploration with systems on the implementation of the National Institute for Clinical Excellence (NICE) accredited interventions to support effective maternity and newborn triage via the 111 and 999 systems within our service will be a focus for 2023/24. NWAS has also supported the appointment of the Consultant Midwife as a senior nurse and midwifery research leader with the National Institute of Healthcare Research (NIHR), focused on building capacity and capability for research within the ambulance sector.
Mental health
During 2022/23 we received 120,870 999 mental health calls. 20.1% of these calls were hear and treat outcomes, 39.3% of these calls were see and treat outcomes and 40.6% of these calls were see and convey to hospital. Over the last 12 months, work has developed to ensure from a mental health perspective patients get the right care.
This work has included:
- Deliver the learning disabilities and autism plan
The learning disability plan has been developed after a period of extensive consultation with staff, system partners and people with autism and learning difficulties. The plan is due to be launched in 2023/24 and will run for three years. The learning disability and autism practitioner post has been substantiated and the post holder will oversee the implementation of the plan and evaluation of its outcomes.
Deliver the mental health plan to ensure equity of response for mental health patients and implement the staff suicide prevention toolkit
Over the last 12 month the focus has been on implementing the aspirations within the NHS long term plan regarding the ambulance response to mental health.
Mental Health Practitioners in EOC
The mental health team continue to work with ICB leads, commissioners and mental health partners to embed a model of mental health practitioners from mental health trusts working in EOC to triage Category 3-5 mental health calls. The aim is for this to be a rotational model whereby the mental health practitioners rotate into EOC, our mental health response vehicles and into their own crisis team. The mental health team are aiming that all areas have an implemented integrated model this year. Areas updates are as follows:
- Greater Manchester: A trial went live in November 2022, with mental health practitioners from Greater Manchester Mental Health Trust and Pennine Care working 12-12 midnight, 7 days a week in EOC Parkway, Manchester. Data to date consistently indicates that the practitioners hear and treat (supporting the patient over the telephone and potentially onward referring into appropriate services) rate is over 50%, thereby preventing an ambulance being dispatched on these occasions, and gaining the correct support for the patients need. This trial is now being developed to look at the role of Greater Manchester Police (GMP) in this model, as approximately, 40% of mental health calls to us are received via GMP; and the role of Voluntary Community and Social Enterprise (VCSE) is being able to signpost lower acuity mental health calls that have been triaged into VCSE service provision for support, to help reduce the likelihood of the individual ringing again. The plan is that this model will become embedded as an integrated model by late spring/early summer 2023, and there is a Greater Manchester steering group that meet fortnightly to provide the oversight, and an internal group who meet monthly. Learning for the GM trial is being used to inform developments in other areas.
- Cheshire and Mersey: In conjunction with Mersey Care, in December 2022, a small trial of one mental health practitioner working in EOC Estuary Point was established for three months, to support with winter pressures. This was on a part time basis working 3 x 13:00 to 23:00hr shifts a week. The data collected for this trail identified that the practitioner had a 73% hear and treat rate thereby, preventing ambulances being dispatched to these individuals. The mental health team are now working with the Mersey Care senior leadership team to agree the long-term model. In Cheshire talks are ongoing with Cheshire and Wirral Partnership to agree and develop the
most appropriate model. Due to the geographical location of the mental health practitioners and EOC Estuary Point, other options/locations are also being explored.
- Lancashire and South Cumbria: The mental health advice line (MHAL) model has been in place operating from EOC Broughton for several years. Work is ongoing with the commissioner and manager of the team to review standard operating procedures and to review team numbers in response to mental health demand.
- North Cumbria: In North Cumbria discussions are ongoing with system partners to agree the most appropriate model considering geographical footprint and call volume.
Staff support and suicide assessment and postvention toolkit
The mental health team provides support to the People directorate with staff health and wellbeing initiatives including representation and provision of expertise in the mental health continuum delivery group. The team will also support managers with advice and guidance on mental health and wellbeing in the workplace and individual staff and provide signposting to the resources that staff can access independently or that managers can use to support staff with their mental health.
- Digital
Our digital work programme has continued to focus on solving everyday problems using digital solutions, implementing new integrated critical systems, ensuring we have safe and resilient digital platforms, providing staff with the information they need to make the best decisions, testing new innovative ideas and developing progressive digital partnerships. We continued with the capital investment plan matched by significant external funding through the Unified Tech Fund to continue to upgrade our infrastructure and devices and enhance key digital programmes of work. Key achievements for 2022/23 included:
Solving everyday problems: We are committed to making sure staff have the basics they need. Station upgrades have taken place across this year with networks being upgraded to 50Mb symmetrical connections and new Cisco switches installed. The migration from EE to O2 has commenced, with the rollout of new SIM’s and handsets where required, and a new
data management system (MODA), which is helping us to monitor data usage more effectively. The Office 365 business case has been developed, which will ensure staff access to the right information at the right time. A dedicated digital training team has been established, supporting staff to use digital tools and applications, including electronic patient record (EPR) Phase 2, the new De-Fib roll out and use of iPads. The service desk team resolved 81% of all incidents and requests between April 2022 – March 2023, and have continued to achieve the target of <1% of re-opened requests.
Our digital journey: Our Smart sites programme has continued to develop over the last year and includes the scale up of digital key cabinets, controlled drugs key solution and digital wallboards. Three new digital innovation support roles have been recruited to, which will support implementation of the new technology as part of Phase 2. Work has continued on Electronic Patient Report (EPR) Phase 2, which includes new mandatory fields, a GP connect viewer and an improved user interface. Our interoperability programme has focused on streamlining patient markers and patient information across three service lines and work with the national team to develop the Booking and referral Standard (BARS) across 999 and
111. A new referrals system for safeguarding referrals into local services has been developed on Cleric and successfully implemented into business as usual. In January 2023, the North West were the first region in the country to go live with DoS road distances, supporting service efficiency and improving patients’ journeys. A further review of NHS Service Finder ambulance referral schemes was undertaken, simplifying the process for front line ambulance clinicians to make referrals and reduce avoidable conveyance. We are also leading pioneering work to enable front line clinicians to utilise the DoS to digitally refer patients direct from scene.
Secure and joined up systems: Server patching and Carecert compliance has increased during the year, and cyber breaches, measurable following implementation of DCIQ, were within the accepted tolerance target (<20) by the end of the year and averaging at 5 per month. Work continues to develop the Ambulance Data Set further, in line with nationally mandated EPR data set items. Having a standard return will allow benchmarking with other ambulance trusts and in the long term, reduce national reporting requirements/burden. We also continued our replacement programme for core infrastructure to make sure our
systems are safe, reliable, and resilient. This was further supported by implementation of quarterly failover for critical systems.
Smarter Decisions: There was a total of 328 Business Intelligence helpdesk requests made during 2022/23, which equates to almost 1.5 requests for every working day of the year. Significant work this year was undertaken by the team to implement the HALO reporting which enables trusts to capture patient cohorting as part of the handover data set. The SafeCheck data set was integrated in our data warehouse, bringing the total number of data sources in the BI Data Warehouse to 10, and 4 new Power BI developments are fully tested and deployed, including IPC, HALO, ICB, and SafeCheck. Approximately 48,000 unique views in Power BI were recorded this year, an average of c.4000 per month. New BI measures will be introduced for 2023/24 which will capture the number of opened FOI BI helpdesk requests, number of Power BI training sessions provided, and number of Power BI new contents approved/published.
Digital Pioneers: We continued to grow several partnerships to support our ambition to be digital pioneers including the University of Manchester, Lancaster University, the Northern Ambulance Alliance and AACE digital transformation group. We continue to chair the Ambulance Digital Innovation forum, providing an opportunity for ambulance trusts to share work and collaborate. A new RFID pilot has begun in Carlisle station to explore how the technology can improve safety check processes. Development work has focused on a new version of SafeCheck (v1.2) which incorporates a range of technical upgrades to improve user experience for operational staff. A new ‘Aspirer’ platform, incorporating digital timesheets and an appraisals module has also been developed. Work has continued on the development of APEX Phase 1 which is due to be completed in quarter 1 2023/24. Our data innovation work has also progressed – we have partnered with Skunkworks AI lab to create an algorithm predicting the outcome of calls to aid the clinical stack and implemented a live RPA process removing the need for a daily report produced by the analyst team. A digital design forum (DDF) evaluation session was held in January summarising activity through the forum during 2022. This has informed work on a re-design the DDF, to help to define some of the processes underpinning it and to clarify roles and responsibilities.
- Patient engagement and experience
Each year we deliver an extensive patient engagement programme in line with our patient public and community engagement implementation plan. The plan sets out the ways we propose to engage with and obtain feedback from our patients across all service areas. A review of all the patient experience receiving of survey feedback and reporting channels and platforms was undertaken to ensure best practice as well as best value. In 2022/2023 the plan also highlighted the flexibility with engagement presented by predominantly using virtual channels to save on travel times and planning attendance with diverse groups in the region, to continue to gather real insights into the care and treatment that patients receive.
A minimum 1% of PTS, PES see and treat, and 1,200 NHS 111 patients receive the opportunity to provide Friends and Family Test (FFT) feedback monthly. In addition, to our NHS 111 postal survey offer and FFT comment postcards on vehicles, we continued to develop our digital offer by offering the opportunity to complete our patient surveys via a text weblink and online via our website. Also, instead of the traditional face to face engagement that would normally take place with patients, health practitioner networks, forums and community groups, in 2022/2023 we attended these across virtual engagement sessions via MS Teams and Zoom.
Positively we have continued to grow and develop our Patient and Public Panel (PPP) and to use their feedback and lived experience to better understand patient experience, produce stories, analysis and themed findings which will inform service development.
Patient and Public Panel – giving our patients a voice
Our volunteer Patient and Public Panel (PPP), established in 2019, is made up of representatives from local communities, interest groups, the voluntary sector and partner organisations, and offers meaningful opportunities for members to influence decisions and identify improvements in our urgent and emergency care, patient transport, NHS 111 and back-office services in a way that suits their lifestyle and the time and commitment they are able to give. Panel members bring expert lived experience and knowledge of our services and offer valuable insights into numerous projects, initiatives, policies, systems and
campaigns. During 2022/23 almost all involvement was undertaken virtually but this is expected to change in 2023/24.
The PPP has a flexible infrastructure to enable patients and the public to become involved at one or more levels that best suit them. All levels are equally important and consist of:
- ‘Consult’ is virtual, making the most of digital channels to interact with members who can get involved whenever or wherever they choose.
- ‘Co-produce’ panel members work together on short-term projects using co- production techniques.
- ‘Influence’ members take an ongoing, active role in high-level meetings to enhance decision making and discussions.
Our PPP has continued to grow, and we have actively engaged the membership via virtual platforms throughout the past 12 months. We now have 268 PPP members fully inducted, with most already involved in our work. We have reached our target for disability (20%) with 29% (77) of the 268 PPP members declaring they have a disability. We also hit our 2022/23 youth target of 25%, with 68 youth members signed up to our PPP membership. Ethnic minority representation at the end of March 2023 was 16% against a target of 30% and we recognise more work needs to be done to continue to engage with diverse communities across the North West. This will be a focus area for us in 2023/24.
From April 2022 to March 2023, PPP members have been invited to get involved in 85 opportunities with 33 requests for panel involvement from staff across the trust.
Patient engagement activities align themselves to our EDI priorities with improving access and experience with hard-to-reach communities. Actions associated with this include targeted engagement with our black and minority ethnic communities with attendance at face-to-face events for example Windrush, Burnley Health Mela and Preston Carnival to name some. Our attendance at these events is also supported by our positive action officers, PPP leads and occasionally operational crews. Here, positively opportunities with recruitment both to our services and voluntary roles are relayed and any support that might be needed for would be applicants is co-ordinated for further attention.
Further patient engagement activities also include hosting listening conversation events in predominately black and minority ethnic community areas of Greater Manchester, Liverpool and Lancashire respectively. Here we can learn and understand more with gaps to our communities accessing our services being delivered and recommendations for improvements are subsequently applied. Some examples of these include tailored literature and information for Mosques, basic CPR training for our deaf communities, launch of the BSL 999 emergency video relay service (999 eVRS) again for our deaf communities and those with speech impairments, a pilot of the ‘Language Line Insight App’ for our frontline operational staff to access language interpretation services whilst at patient side. A further outcome of this work includes over 30% of our young Patient and Public Panel (PPP) members have been recruited from our black and minority ethnic communities.
Areas the PPP have been involved in include regular attendance at high-level meetings such as area learning forums, attendance at Board and learning from deaths. PPP members have been involved in various projects, including hospital handover improvement collaborative events, taxi in 5 project, cardiac arrest project research, palliative care research, PTS Public Health awareness project along with providing comments and feedback on the introduction of NHS Pathways into Emergency Operational Centres.
The panel membership receives regular information via a weekly roundup newsletter and quarterly bulletin, opportunities to engage with each other on a dedicated PPP members area including the Ambulance Academy for young persons and virtual development sessions (CPR, mental health and safeguarding). They have also had the opportunity to provide feedback on key documents and publications such as our winter campaign.
We are very proud of our volunteers and their achievements and in 2022/2023, a PPP achievements summary book was produced in recognition of the panel’s third year anniversary. We are currently in the early planning stages of planning a face-to-face PPP celebration event in the early summer of 2023/24 to thank our PPP members for their continuous support and celebrate many achievements, something which has not been possible during the pandemic period.
A breakdown of PPP member’s involvement by level can be found at Figure 9.
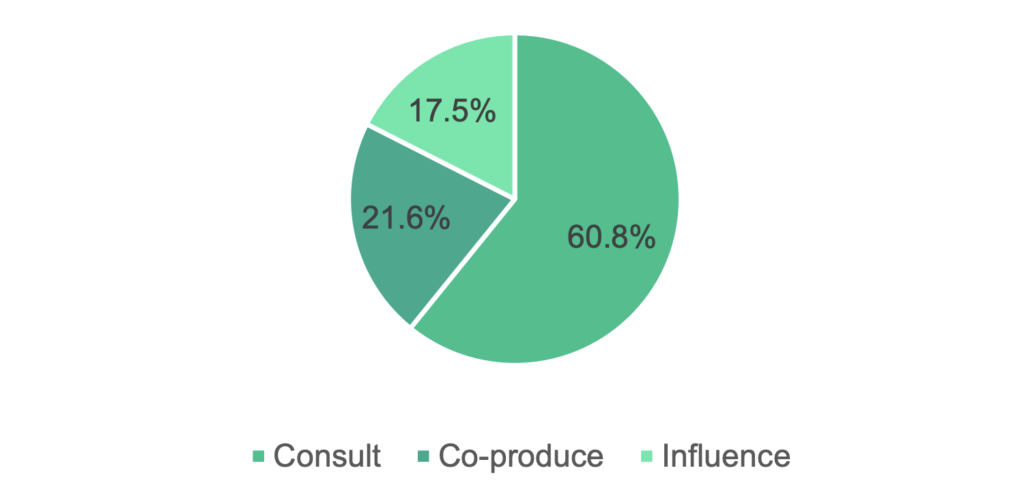
A breakdown of PPP members by age can be found at Figure 10.
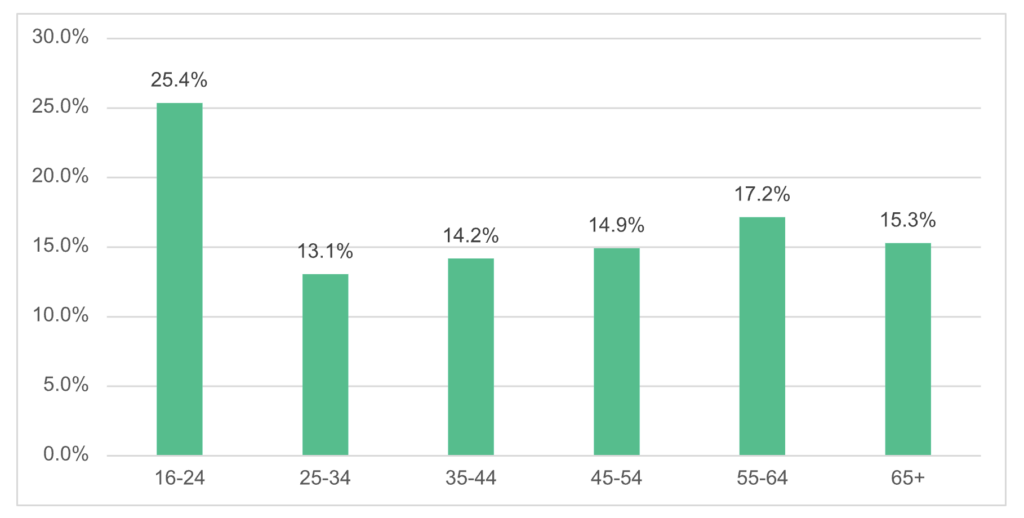
Patient feedback including Friends and Family Test 2022/23
An extensive patient engagement programme was successfully completed during 2022/23. In addition, to our NHS 111 postal survey offer and Friends and Family Test (FFT) comment/postcards on vehicles, we continue to develop our digital offer by offering the opportunity to complete our patient surveys via a SMS text weblink and online https://www.nwas.nhs.uk/get-involved/share-your-experience/tell-us-how-we-did/ Also, instead of the traditional face to face engagement that would normally take place with
patient, health practitioner networks, forums and community groups, in 2022/23 we attended these via MS Teams and Zoom.
FFT national reporting has a continued focus on digital channels via text. Figures 11 and 12 below respectively provide a summary of survey response feedback data including FFT by quarter.
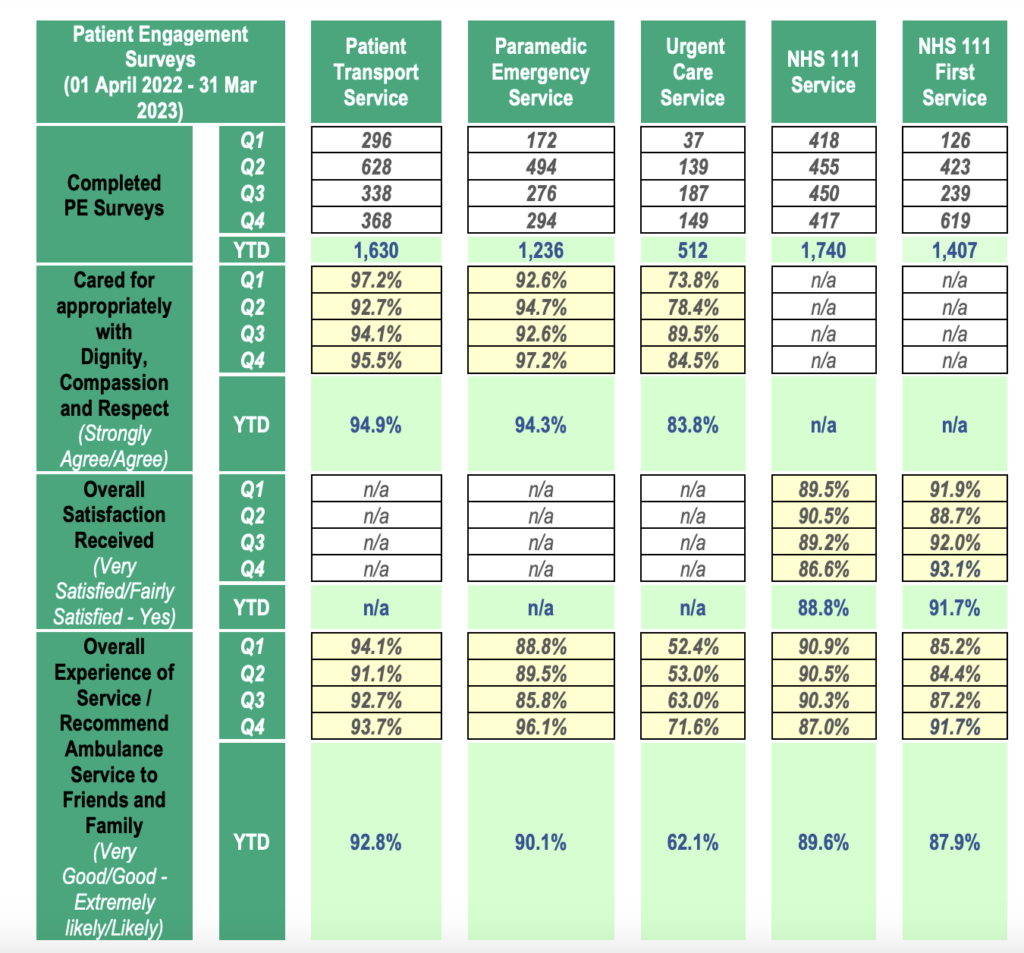
In summary, for the 2022-2023 year we received:
- 18,607 survey responses, 3.67% more than the previous year
- 14, 625 comments supported these surveys
- 99.94% of responses came via text message
- 0.05% were sent in via the post
- 0.01% were sent via an online survey
Patient public and community engagement
Whilst patient surveys provide us with a real insight into the care and treatment that patients have received, another method we use to gain qualitative feedback is by engagement with community and patient groups within our region – as mentioned above this has continued to take place virtually during most of the last year. Our focus has been to reassure communities that they are safe using ambulance services as we moved out of the Covid-19 years and reaffirm the basics of what we offer across each of our 3 main service lines.
More than 43 virtual engagement events were attended by the team as either principal speakers, advisory or facilitators. Some examples include Lancashire Learning Disability Partnership Board, CLP Patients, Public and Carers Voice Forum Meeting, Cumbria Deaf Association, Healthwatch Wirral, Healthwatch Sefton, NCompass, Insight Healthcare, Caribbean and African Health Network.
Feedback themes
Feedback has fluctuated over the year but has consistently demonstrated a general high regard for the ambulance service and in particular the high percentages of patients feeling they were treated with dignity compassion and respect.
Themes during this period have included:
- Constraints and pressures that we have continued to work under as we moved out of lockdown – both as an ambulance service and part of the wider healthcare sector. The public recognise that it is not always the ambulance service’s fault when we are delayed getting to patients.
- The impact of the cost-of-living and energy costs with mental health related calls, and secondly whether that will impact on us being able to run ambulances.
- Job roles within the ambulance service.
- Ambulance service understanding of young onset dementia.
- PTS criteria including use of escorts and whether PTS staff/volunteers are still required to wear PPE.
- Accessing services for both ethnic minority and deaf communities.
- Lack of awareness of NHS 111 online, mental health support provision, safeguarding and referral processes.
- Reassurance that we can still provide cover on industrial action days.
Positively we are now also seeing the return of large-scale face to face community events and have been able to attend 12 in 2022/23. Face to face engagement with students and others at Freshers Fayres has particularly helped with the recruitment of more young people to our Patient and Public Panel as well as help inform the development of the newly introduced online resource: Ambulance Academy.
We will continue to build on our face-to-face attendance during 2023/24 as Health Melas, PRIDE and other high footfall events are back on the events calendar.
During 2022/23, we have also delivered 5 placed based face to face Community Conversation events of our own. These were successfully first introduced in 2019 but were then paused during the pandemic. Events have been well attended with attendees from a range of public, patients and communities. A key focus for this type of engagement was to listen to, elicit feedback, reassure, and answer questions or concerns raised by our North West communities on our services. Attendees hear from service themed ‘lightning
speakers’ before taking part in short interactive table exercises that helps us identify what we are doing well as well as what needs to be improved. A summary of feedback and what is to be changed as a result is produced and shared with attendees as well as community and specialist patient groups across our North West footprint.
Recommendations for improvements
Our engagement activities with patients, the public and communities allows us to identify specific themes, these are supported by survey feedback which are further analysed and articulated as recommendations for improvements. Some of these include:
- Feedback from our deaf community has highlighted the increased barriers to accessing 999 services. As a result, we launched the 999 BSL Video Relay service in June 2022. We also piloted an ‘Insight’ language communication App for operational staff to download on their iPads.
- We provided reassurance to our patient, public and community groups post pandemic regarding resources, safety of our services, availability and our overall response via regular stakeholder updates, patient engagement events and information bursts. We also kept them informed on an area-based perspective of the availability of local services to support their self-care, with mental health as well as physical health and well-being respectively.
- Learning dashboards shared with PTS services lent support to purchasing bariatric wheelchairs for our PTS Ambulances as well as a review of hospital site maps for patients and staff to navigate and access hospitals easier.
- Further to feedback at the Lancashire community conversation event, we also developed posters and PPP information specific to Mosques and translated our winter watch leaflets into the top languages requested in 2022/23.
- Following receipt of PPP input into the review of our ‘Faith and Culture Card’, a ‘new’ version will be made available electronically as part of the Directory of Services information inclusive of how to support differing communities at the time of a death.
- Funding has been received further to co-production work with the PPP on a new digital version pictorial communication handbook for staff to upload on to new iPads. Consideration will be provided to similar with a digital version of the Multi Lingual Phrasebook to further enhance communication with ethnic minority ‘new’ communities in the region.
- FFT data and thematic dashboards will support co-designed improvements with PTS, PES NHS 111 ambassadors.
- Following feedback that we need to make our PPP sessions more accessible to younger persons we have ensured that our PPP sessions are inclusive by having them hosted virtually at different times of the day. This supports our younger panel members that may have enrolled classes at colleges and universities during the day and for those panel members that work at different times.
- A recite me function on our website ensures publications such as the Ramadan Guide 23 is more accessible for disability and language needs. The PPP weekly roundup and monthly info bursts are now also provided in an accessible format for our visually impaired members and those who require their information in high contrast.
- We also have also invested in a photo symbols subscription so we will be able to produce more easy read information in the future. Monthly newsletter support will be continued throughout 2023/24 for our PPP membership.
- Our recent review of the patient engagement reporting platform we use to store and analyse patient feedback supports North West areas, towns and cities based understanding with patients’ survey feedback and well as by demographics.
7.7 Pillars of quality
We improve quality continuously using our ‘pillars of quality’ listed below:
- Complaints and Compliments
- Incident reporting and learning (including serious incidents)
- Safeguarding
- Health, safety, security, and fire
- Infection prevention and control
- Medicines management
7.7.1 Complaints and compliments
In October 2022, we implemented the new Datix Cloud IQ (DCIQ) system. This system is used to capture incidents, near-misses, good care and outcomes across the organisation. DCIQ better assists in identifying themes, trends and learning due to improved and meaningful data fields, versus the number of free text fields in comparison to the legacy DatixWeb system. As the new incident reporting system was introduced part way through the year incidents data has been summarised separately. This reporting change is also reflected in the incidents, serious incident and health, safety, security and fire 2022/23 data summaries.
Management of complaints & enquiries
We welcome all feedback from patients, including those whose experiences have not met their expectation and so have raised this with us through the complaints process. The complaints we receive offer a unique opportunity to investigate what has happened and where necessary, identify and implement lessons learnt. This can be at an individual and/or a system wide level. Providing a timely compassionate resolution and response to our complainants is one of our core priorities.
There is robust assurance around the monitoring and management of complaints. The Board of Directors receive information on complaints through a monthly integrated performance report. This is supported by assurance reports submitted to the Quality and Performance Committee quarterly, and the Commissioner and ICB joint meetings with our Quality and Safety(Q&S) Group and Regional Clinical Quality Assurance Committee (RCQAC) Area Learning Forums monitor actions arising from complaints via associated action plans and the NHS 111 service complaints are reported through the NHS 111 governance reporting procedures.
In 2022/23, we received 2,028 complaints in total.
April to October 2023 data reported via DatixWeb
In DatixWeb, 994 complaints were reported (01 April 2022 till 03 October 2022) this is broken down by risk score:
- Risk Score 1: 326
- Risk Score 2: 515
- Risk Score 3: 127
- Risk score 4: 17
- Risk Score 5: 9
Of the 944 complaints, the table below identifies the categorisation and total number.
| Complaints by Type | Number of Complaints |
| Staff Conduct | 214 |
| PTS Journey Times | 208 |
| Emergency Response Delays | 205 |
| Care & Treatment | 193 |
| Communication & Information | 109 |
| Driving Standards | 39 |
| Damage or loss to property | 16 |
| End of Life care | 1 |
| Safeguarding | 1 |
| Not categorised | 8 |
| Total | 994 |
Table 11: Complaints summary 2022/23 Datix Web
October 2023 to March 2023 data reported via DCIQ
In DCIQ, 1,034 complaints were reported (03 October 2022, till 31 March 2023). This is broken down by risk:
- Low Risk (formerly Risk Score 1 & 2): 902
- Medium Risk (formerly Risk Score 3): 104
- High Risk (formerly Risk Score 4 & 5): 28
Of these 1,034 complaints, the table below identifies the categorisation of complaints and total number.
| Complaint Category | Number of Complaints |
| Accidents & Injuries | 5 |
| Call Handling | 152 |
| Care & Treatment | 390 |
| Communication | 76 |
| Damage | 22 |
| Delays | 393 |
| End of Life/ Palliative Care | 1 |
| Equipment Non-Clinical | 1 |
| Infection Prevention & Control (IPC) | 1 |
| Information Governance | 2 |
| Medicines Controlled Drugs | 1 |
| Moving and Handling | 18 |
| Road Traffic Incident | 6 |
| Security | 1 |
| Slips, Trips & Falls | 2 |
| Vehicle | 4 |
| Violence & Aggression | 5 |
| Welfare | 9 |
| Total | 1089* |
Table 12: Complaints summary 2022/23 DCIQ
*Number is higher as some complaints had more than one complaint category associated with it.
DCIQ allows us to scrutinise this data more closely, and for the top 3 types, we can explore the sub categories of each where this has been populated.
| Complaints by Type | Sub-Type | Number of Complaints |
| Delays | Response Times: Resourcing | 182 |
| Access to Emergency Department | 10 | |
| NWAS Call Pick up | 5 | |
| Response Times: Navigation Systems | 2 | |
| Access to PPCI | 1 | |
| Safe Discharge | 1 | |
| Access/Egress | 1 | |
| Waiting for Police Attendance | 1 | |
| Care & Treatment | Professional Standards (Originally Conduct in Datix Web) | 249 |
| Advice given by NWAS | 58 | |
| Treatment provided by NWAS | 28 | |
| Referral from NWAS | 22 | |
| Equality: Language | 2 | |
| Safeguarding | 1 | |
| Clinical Records | 1 | |
| Arrangements after Patient’s death | 1 | |
| Confidentiality | 1 | |
| Call Handling | Professional Standards | 43 |
| Advice given by NWAS | 30 | |
| Call Handling timeframes | 28 | |
| Call Referral | 28 | |
| Eligibility Criteria | 6 | |
| Audit | 3 | |
| Information Gathering | 2 | |
| Escalation | 2 | |
| Call Termination | 2 | |
| Patient Demographics | 2 | |
| Total | 712 |
Table 13: 2022/23 top 3 complaints detailed summary taken from DCIQ
The breakdown of complaints by geographical area.
| Geographical Area | Number of Complaints |
| Cumbria & Lancashire | 272 |
| Cheshire & Merseyside | 318 |
| Greater Manchester | 498 |
| No Value | 1 |
| Total | 1089* |
*Number is higher as some complaints had more than one complaint area associated with it.
The breakdown of complaints by service line.
| NWAS Service Line | Number of Complaints |
|---|---|
| PES | 297 |
| PTS Bureau | 237 |
| Emergency Operations Center | 203 |
| NHS 111 | 184 |
| PTS Operations | 158 |
| Clinical Hub | 3 |
| PTS Central Rostering Unit | 2 |
| NWAS | 1 |
| North West Air Ambulance | 1 |
| PTS Assurance | 1 |
| No value | 2 |
| Total | 1089* |
*Number is higher as some complaints had more than one complaint service line & category associated with it.
Complaint Outcomes
We have an agreed Redress Procedure to provide guidance on questions of remedy in line with the guidance provided by the Parliamentary and Health Service Ombudsman (PHSO) for reasonable, fair and proportionate remedies during its complaints handling processes. For 2022/23 the outcomes of complaints investigated by the Patient Safety team were as shown below with the percentage of the total complaints received shown below:
| Upheld | Partly Upheld | Not Upheld | Ongoing |
| 378 | 515 | 980 | 112 |
| 19% | 26% | 49% | 6% |
Compliments
1507 compliments were received and processed during 2022/23 from across all service lines within our geographical footprint. This was an increase of 97 compliments on the 2021/22
figure. Work has continued with the Datix Cloud IQ system to embed it fully and to further explore its functionality to enable us to compare and share information about compliments and promote learning.
7.7.2 Incident reporting (including all serious incidents)
Reporting, monitoring, acting on, and learning from patient safety incidents is a key responsibility of any NHS provider. We actively encourage all our people (staff and volunteers) to report incidents and near-misses so that we can learn when things go wrong, make improvements, and share learning when things go well.
We review all incidents and takes any immediate actions identified and considers safeguards for patients and our people.
We externally report all unintended or unexpected patient safety incidents which could or did lead to harm via the NHS National Reporting and Learning Service (NRLS). Themes and trends from all incidents, including serious incidents are reported quarterly to the Quality and Performance Committee and via the Chairs Assurance Report to the Board of Directors.
In 2022/23, there were 13,438 incidents in total.
In DatixWeb 7,215 incidents were reported (01 April 2022 till 04 October 2022) this is broken down by risk score:
- Risk Score 1 (Low): 825
- Risk Score 2: 4,445
- Risk Score 3: 1,739
- Risk Score 4: 111
- Risk Score 5 (High): 15
80 incidents reported were rejected.
The table below identifies the categorisation of the 7,215 incidents:
| Incidents by Type | Number of Incidents |
| Raise an issue/ concern | 1,971 |
| 111 | 1,628 |
| Staff injury | 1,007 |
| Clinical incident | 692 |
| Raise a notification | 507 |
| Road Traffic Collisions (RTC) | 345 |
| Non-clinical incident | 302 |
| Clinical near miss | 280 |
| Non-clinical near miss | 191 |
| Patient injury | 185 |
| IM&T and IG Security | 89 |
| Public injury | 18 |
| Total | 7,215 |
Table 17: Incident type 22/23 Datix Web
In DCIQ, 6,223 incidents were reported (04 October 2022, till 31 March 2023). This is broken down by risk score:
- Risk Score 1 (Low): 2,647
- Risk Score 2: 2,257
- Risk Score 3: 1,069
- Risk score 4: 137
- Risk Score 5 (High): 108
5 incidents reported were rejected.
Of these 6,223 incidents, 2,953 pertain to a patient event, 2,222 to a staff event and 1,048 to a trust event. The table below identifies the categorisation of incidents and total number.
| Incidents by Type | Number of Incidents |
| Call Handling | 787 |
| Delays | 713 |
| Care and Treatment | 652 |
| Communication | 558 |
| Violence and Aggression | 583 |
| Accidents and Injuries | 505 |
| Road Traffic Collision (RTC) with Vehicle | 280 |
| Medicines: General | 272 |
| Damage | 220 |
| Call Management | 170 |
| Medicines: Controlled Drugs (CDs) | 153 |
| Road Traffic Collision (RTC) with Object | 147 |
| Equipment: Clinical | 140 |
| Equipment: Non-Clinical | 115 |
| Welfare | 109 |
| Slips, Trips and Falls | 105 |
| Moving and Handling | 96 |
| Maternal, Obstetric & Neonatal | 93 |
| Infection, Prevention, & Control | 92 |
| Security | 77 |
| Information Governance | 71 |
| Vehicle | 71 |
| External Organisation Enquiry | 49 |
| ICT | 41 |
| Cyber Security | 33 |
| End of life | 33 |
| Mental Health | 29 |
| Estates and facilities management | 15 |
| Road Traffic Collisions | 7 |
| Fire | 6 |
| Surgical Interventions | 1 |
| Total | 6223 |
We co-operate with any externally managed investigations conducted by the Healthcare Safety Investigations Branch (HSIB) or the Care Quality Commission (CQC). These organisations request information from us to support their ongoing investigations and this is overseen by the Patient Safety team. Information requests from these organisations are shared within fourteen calendar days.
During 2022/23, we received 13 formal requests from HSIB and 7 from the CQC. The areas of focus for 2023/24 will be to:
- Continue the proactive engagement on encouraging timely event reporting (incidents, near-misses, good care and outcomes) via the DCIQ system.
- Ensure events are initially triaged and allocated for review within 72 hours of reporting.
- Provide a professional advisory and support service to meet and continuously improve closure and feedback timescales.
- Provide a support service to ensure high quality feedback to event reporters to enhance our commitment to promoting a just and safe culture, where it encourages our people to report events.
- Transition from national reporting from NRLS to Learning from Patient Safety Events (LFPSE)
External incidents
External incidents are categorised as issues, concerns, or feedback provided by partner agencies or the wider health and social care economy regarding the care that has been provided by our service. Whilst these incidents do not meet the same strict guidelines for the management of a complaint raised by a patient, relative or person acting on behalf as specified in the NHS Complaints Regulations 2009, we recognise the learning opportunities that can be drawn from these incidents as well as assisting with maintaining a collaborative, and professional working relationship with our partner agencies and key stakeholders.
During 2022/23, 1,820 external incidents were received. The table below shows the number of external incidents received by quarter.
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 2022/2023 | 360 | 253 | 600 | 607 | 1,820 |
In addition to external incidents coming into the trust, we equally raise incidents to external agencies and health and social care organisations.
During 2022/23, we raised 977 external out incidents. The table below shows the number of external out incidents by quarter.
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 2022/2023 | 203 | 275 | 322 | 177 | 977 |
Serious incidents
Serious incidents are reported in line with the NHSE SI Framework (2015), and an in-depth comprehensive investigation is completed to identify learning and any actions. The aim of serious incident investigations is to establish the facts of the event that has occurred and includes, what happened, to whom, when and where. Once the facts have been established the investigation will seek to establish the reasons why the event occurred, including contributory factors. This methodology is used to identify learning and improvements rather than apportion blame and systems are reinforced to effectively reduce the likelihood or eliminate recurrence in the future.
Every SI investigation is shared with our lead commissioner for review and presented to either the Quality and Safety Group or the Regional Clinical Quality Assurance Committee (RCQAC) to provide assurance on the quality of the investigation, robustness of the action plan and that learning is identified prior to formal closure of the serious incident.
An event that meets a risk score of 4 or 5 will be subject to a 72-hour review (case assessment) and presented at the next Review of Serious Events (ROSE) meeting, chaired by the Medical Director, for assessment as to whether the event meets any of the criteria of the Serious Incident (SI) Framework and therefore is required to be reported on the Strategic Executive Information System (StEIS) database to NHS England and our lead commissioner within two working days of the SI being declared.
The ROSE meeting takes place weekly, and the membership comprises of a diverse range of senior clinicians across our services, subject matter experts and a patient representative to provide a patient perspective as part of the process.
During 2022/23, a total of 373 cases were reviewed at the ROSE meeting. On some occasions, cases are presented on more than one occasion to the ROSE meeting when further information is requested before a decision is reached about whether the case meets the SI criteria. 100 of those cases were deemed to meet one of the criteria under the Serious Incident Framework, and subsequently reported on Strategic Executive Information System (StEIS) within the compulsory 2 working day timeframe.
The below table compares the number of Serious Incidents over a three-year period.
| Year | Q1 | Q2 | Q3 | Q4 | Total |
| 2020/2021 | 13 | 12 | 15 | 10 | 50 |
| 2021/2022 | 10 | 18 | 23 | 35 | 86 |
| 2022/2023 | 18 | 18 | 24 | 42 | 100 |
A thematic analysis undertaken into the SIs declared identifies the following areas:
- Delays: an ambulance response was delayed to the patient
- Care and Treatment; the care provided to patients by our people
- Call Handling/ Management; unsafe or inappropriate processing of calls
- Medicines; administration errors and/ or security weaknesses with medicines
- Mental Health; patients with mental health presentations.
The breakdown of SIs by location and service is detailed below.
| Geographical Location | Number of SIs |
| Cumbria & Lancashire | 36 |
| Cheshire & Merseyside | 36 |
| Greater Manchester | 28 |
| Total | 100 |
| NWAS Service Line | Number of SIs |
|---|---|
| Emergency Operations Centres (EOC) | 69 |
| Paramedic Emergency Services (PES) | 26 |
| Patient Transport Services (PTS) | 2 |
| NHS 111 Service | 2 |
| Trust-wide | 1 |
| Total | 100 |
During 2022/23, there have been occasions when a SI has occurred which directly involved the trust and other provider organisations. We are committed to ensuring timely and collaborative working with other organisations and agencies involved to undertake a combined investigation, where this is appropriate.
As part of the NHS Patient Safety Strategy 2019, and planned changes to the management of serious incidents, we have been strengthening our processes to improve the timeliness of initial reviews and learning, with increased early engagement of professionals, patients and their families using a restorative, just and learning culture approach. The initial feedback from those involved, including those affected by a serious patient safety incident has been positive.
The areas of focus for 2023/24 will be to:
- Continue with the running of the existing Serious Incident Framework until we are ready to transition to the new Patient Safety Incident Response Framework (PSIRF).
- Continue to provide a professional serious incident investigation function to meet and continuously improve investigation timescales.
- Develop collaborative working relationships with health and social care organisations to undertake combined serious incident investigations, when appropriate.
- Provide a professional advisory and support service pertaining to serious incident investigations and lead the change in using the System Engineering Initiative for Patient Safety (SEIPS) Framework to look for interactions rather than simple linear cause and effect relationships.
Regulation 28
We received one Regulation 28 report from HM Coroner in 2022/23. We aim to receive a very low number of Regulation 28 reports as it proactively and continuously seeks opportunities for improvement and to ensure that any/all learning actions which may arise from a coroner’s investigation are completed in a timely manner.
Never events
Never events are a sub-set of serious incidents and are defined as serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented by healthcare providers. There were zero never events during 2022/23, and in previous years.
- Safeguarding
We have a statutory responsibility to safeguard children and adults who are at risk of harm from abuse or those who are vulnerable, this commitment is underpinned by specific
legislation, namely Children’s Act (1989 & 2004) and the Care Act (2014). We work in partnership with other organisations to ensure that the response to individuals who are at risk of harm from abuse or neglect or who are vulnerable, is communicated in an effective manner which results in an appropriate response.
Safeguarding activity
2022/23 has seen safeguarding figures fluctuate during the early part of the year, this has been attributed to the Covid-19 pandemic. In November we moved from the ERISS system onto a new referral system through Cleric. This now allows staff to determine whether
referrals are ‘safeguarding or ‘early help’. As seen in the figures this move has caused a significant drop in the number of referrals being made but this is attributed to the fact that crews can make improved judgement on the type of help needed and other pathways now in place such as mental health. The new system has also had fewer rejections by social care than the ERISS system which also suggests that the new referral process is more accurate alongside the additional training staff have received prior to the move to Cleric.
The table below details the activity:
| Concernraised | Apr-22 | May-22 | Jun-22 | Jul-22 | Aug-22 | Sep-22 | Oct-22 | Nov-22 |
| Adult | 4402 | 4512 | 4208 | 4184 | 4392 | 3989 | 4198 | 1868 |
| Child | 794 | 965 | 906 | 848 | 846 | 825 | 747 | 353 |
| Total | 5236 | 5477 | 5114 | 5032 | 5238 | 4814 | 4945 | 2221 |
Table 24: ERISS Safeguarding activity 2022/23 (1st April 2022 – 15th November 2022)
| Concernraised | Nov-22 | Dec-22 | Jan-23 | Feb-23 | Mar-23 |
| Adult SG | 284 | 447 | 460 | 431 | 461 |
| Adult EH | 1088 | 2036 | 1884 | 1597 | 1806 |
| Child SG | 254 | 297 | 405 | 428 | 455 |
| Child EH | 118 | 92 | 128 | 117 | 130 |
| Total | 1744 | 2872 | 2877 | 2573 | 2852 |
Table 25: Cleric Safeguarding activity 2022/23 (10am, 15 November 2022 – 31 March 2023)
Work undertaken in 2022/23
The following areas of work have progressed in the last 12 months:
- Continuing work with private providers to gain assurance in relation to safeguarding, reflecting training, Disclosure and Barring Service (DBS) compliance, policies and procedures and governance.
- Our Support Centre were all trained on use of the Cleric system during 2 days of intensive training. Regular meetings are held to monitor the system.
- All safeguarding and maternity alerts are now placed onto the Cleric system.
- Four bespoke safeguarding/early help forms have been designed in collaboration with social care partners and are now used as part of the new system.
- Safeguarding e-learning packages have been reviewed and rewritten and developed and are now live. Induction pack updated.
- Missing and absconded patients’ procedure introduced in 2022.
- Domestic Abuse procedure and Allegations against staff policy updated.
- Go live of Cleric for all adult and child social care services in October 2022.
- Review of level 3 training and presentation with a back-to-basics approach. Training needs analysis reviewed in line with Intercollegiate document for 2023/24 roll out. Increased numbers of staff will need level 3 safeguarding training in line with the ICD who have not previously had level 3.
- Safeguarding Champions were recruited to assist with rollout and awareness raising of the new Cleric Safeguarding System. The Champions also had an opportunity to share how they felt the new system had been received and embedded. 13 Champions attended a review meeting 4 months after implementation in which feedback was overwhelmingly positive with the highlight being the new ability to raise Early Help requests.
- The Safeguarding Manager left the service in November 2022 and a vacancy for a new Head of Safeguarding is currently being recruited. We expect this post will be in place in July 2023.
Safeguarding systems review
With the continually increasing safeguarding numbers a review of the current systems used was necessary. ERISS (the previous system used) is expensive to maintain and develop further, a working group was setup to review this and operated under the title of Project Emerald.
Project Emerald has seen the start of a whole system change from the electronic referral information sharing system (ERISS) system to the Cleric system. This rollout of phase 1 commenced in November 2022. The Cleric system will allow for more accurate data collection and reporting and will allow the Safeguarding team to monitor rejections and
feedback in a more accurate manner. Work is ongoing to archive the information on ERISS. Cleric has been well received by social care partners.
Safeguarding board engagement
Increased notifications, improved visibility and Board engagement has resulted in increased numbers of requests to be involved in Safeguarding Adult Reviews, Domestic Homicide Reviews, Serious Case Reviews, Learning Disability Reviews and Strategy Meetings.
The Safeguarding team work alongside senior managers and clinicians to ensure engagement with the Boards is visible and specific to local needs. There are currently 46 safeguarding boards across the geographical footprint of North West Ambulance Service and the team have committed to attend each board a minimum of once per year, or, as per local board request. Board engagement is monitored by the Safeguarding team. In addition, practitioners and managers are involved in local safeguarding board sub-groups.
Engagement includes:
- Child Death Overview Panel
- Rapid Response meetings
- Alternative Life-Threatening Event meetings
- Brief Learning Reviews
- Serious Case Review groups
- Safeguarding Adults Review groups
- Domestic Homicide Reviews
- Front line visits with local board members
- Wider stakeholder meetings
- Integrated Care System meetings
- Multi-agency review meetings following the Sudden Unexplained Death of a Child (SUDC)
- MAPPA (Multi Agency Public Protection) Meetings
- Section 42 enquiry meetings.
- High Risk Patients review meetings.
Serious case reviews, safeguarding adult reviews and domestic homicide reviews
During the 2022/2023 year the safeguarding team were involved in 254 safeguarding reviews, these are broken down into 127 adult reviews, 83 child reviews and 44 domestic homicide reviews. In direct comparison 2020/21 saw the team engaged in 229 safeguarding reviews. The safeguarding team will continue to analyse cases and data to identify any themes or learning.
Learning is captured for each organisation involved within the individual reports where applicable. Any learning specifically for us or that can be applied to the trust is recorded as part of the individual report and on the Safeguarding workplan. Learning for these cases is then disseminated through the corporate learning forum, the regional learning forums, directly with the staff involved and trust wide via the weekly regional bulletins and built into the mandatory training scenarios.
- Health, safety and security
We are committed to ensuring a safe system of work approach to health, safety, and security (HSS) and has put in place the organisational arrangements necessary to fulfil its statutory and mandatory obligations. We look to prevent workplace/related injuries, ill health and protection of staff, property, and assets by promoting good working practices. All staff are responsible for ensuring that they follow policies and procedures to keep themselves and their colleagues and patients safe at work. Our HSS work is done in partnership with trade unions who are full members of the sub-committee and work with service lines on local health and safety management.
NHS trusts health safety and security systems are regulated by:
- Care Quality Commission (CQC): It is an executive non-departmental public body of the Department of Health and Social Care established in 2009 to regulate and inspect health and social care services in England and works closely with the HSE with both regulators taking lead for certain issues across NHS trusts. In England,
where providers are registered with them, the CQC is the enforcing authority for patient and service user health and safety.
- Health and Safety Executive (HSE): The HSE is the national independent regulator for health and safety in the workplace. This includes private or publicly owned health and social care settings in Great Britain. The HSE works in partnership with co- regulators in local authorities to inspect, investigate and where necessary take enforcement action.
- Medicines and Healthcare products Regulatory Agency (MHRA): The MHRA is an executive agency of the Department of Health and Social Care; responsible for ensuring that medicines and medical devices work and are acceptably safe.
- Home Office: The Home Office is the lead government department whose responsibilities include fire prevention and rescue. The Regulatory Reform (Fire Safety) Order 2005 applies to all on-domestic premises in England and Wales.
RIDDOR reporting rates in ambulance services
National RIDDOR reporting requires the activity to be reported using the methodology of number of incidents per 1,000 staff. The number of staff employed as at 31/12/2022 is 7037; and the number of staff injury RIDDORs reported in the 12 months to 31 March 2023 is 114 (1.6% of staff). The total number of journeys (PTS (1,327,799) and PES (1,273,189)) combined is 2,600,988 for the same period. The incident rate of RIDDOR reporting is calculated as 16.2 per 1,000 staff members a reduction of 0.7 from 2021/22. The rate of incident reporting per 1,000 staff members in previous years is described in the table below. The incident rate is calculated as 0.04 staff injuries per 1,000 staff journeys. The national RIDDOR comparison rate for 2022/23 is not available at the time of writing this report, and in its absence for the purposes for this report the 2020/21 ambulance sector averages are as follows for comparison.
| Ambulance Sector Average 2020/21 | NWASRIDDOR rate 2021/22 | NWAS RIDDORrate 2022/23 |
| Incident Rate (Injuries x 1000 ÷ No of Journeys) Staff injuries only | 0.11 | 0.05 | 0.04 |
| Incident Rate (Injuries x 1000 ÷ No of Employee) Staff injuries only | 19.38 | 17.5 | 16.2 |
Table 26: Comparison of RIDDOR incident rate Ambulance sector average 2020/21 against NWAS RIDDOR rate 2022/23
Our incident reporting system transitioned from DATIX to DCIQ mid 2022/23. The transition has impacted the data collection for 2022/23 due to differences in data entry methodology between the two systems.
Non-clinical incident activity
DATIX methodology: A non-clinical incident is identified as any incident recorded in the incident reporting system categorised in any of the following categories:
- Raise a concern
- Raise a notification
- Staff injury
- Patient injury
- Public injury
- Non-clinical incident
- Non-clinical near miss
DCIQ Methodology: A non-clinical incident is identified as any incident recorded in the incident reporting system categorised in the following way:
- Accident and injury
- Equipment: nonclinical
- Fire
- Moving and Handling
- Security
- Slips Trips and Falls
- Violence and aggression
The table below summarises the non-clinical incidents reported for the 12 months to 31 March 2022. The non-clinical incident data can be described at directorate level to October 2022, and is grouped more broadly for the second part of 2022/23.
Following several years in growth of reporting non-clinical incidents the position on 31 March 2023 suggests there has been a reduction in incident occurrence as reporting levels have diminished by 30% from 2021/22. There are several factors as to why reporting culture appears to have changed including:
- Non-clinical incident reporting increased significantly during the Covid-19 pandemic years, and this may be a return to non-pandemic reporting levels.
- Non-clinical incident reporting fatigue.
- Staff may not be categorising incidents in the way the DCIQ development team
anticipated, and incidents are ‘lost’ within the new categorisation methodology.
It is likely that the resulting apparent reduction of non-clinical incident reporting is multi- factorial including additional factors to those described above.
| Non-clinical incidents byDirectorate | Q1 2022/23 | Q2 2022/23 | Q3 2022/23 | Q4 2022/23 | Total |
| Service Delivery Directorate (PES, EOC, UCS, PTS etc.) | 2109 | 1991 | 1230 | 1248 | 6578 |
| Medical Directorate | 23 | 28 | 51 | ||
| Finance Directorate(Finance/Fleet/Estates etc.) | 21 | 14 | 35 | ||
| Quality Directorate | 8 | 4 | 12 | ||
| People Directorate | 4 | 9 | 13 | ||
| Corporate Affairs Directorate | 3 | 2 | 5 | ||
| Strategy, Partnership and Transformation Directorate | 4 | 3 | 7 | ||
| Unclassified by Directorate | 271 | ||||
| Trust Workshops | 2 | 2 | |||
| Area Offices | 33 | 30 | 63 | ||
| Total | 2443 | 2051 | 1265 | 1278 | 7037 |
Table 27: Non-clinical incidents by Directorate Q1 & Q2 2022/23. Non-clinical incidents by Business Area Q3 & Q4 Data source: Datix & DCIQ last accessed 18/04/2023. Please note we moved to DCIQ between Q2 and Q3.
Each directorate is expected to review the nature of these incidents at the appropriate level of scrutiny and themes fed through as learning and as part of the Directorate chair report to the Health, Safety and Security sub-committee.
Violence and aggression
We find deliberate violence and aggression towards our staff or people who use our services unacceptable. Where violent or aggressive behaviour may occur due to clinical and or medical factors, all possible primary and preventative measures should be used to reduce the prevalence and risk of harm. Patient facing staff (including 111) have reported 1,188 incidents of violence and aggression in 2022/23, a reduction of 24% (2021/22: 1,567 incidents) and this unexplained reduction may be because of the multifactorial rationale mentioned above.
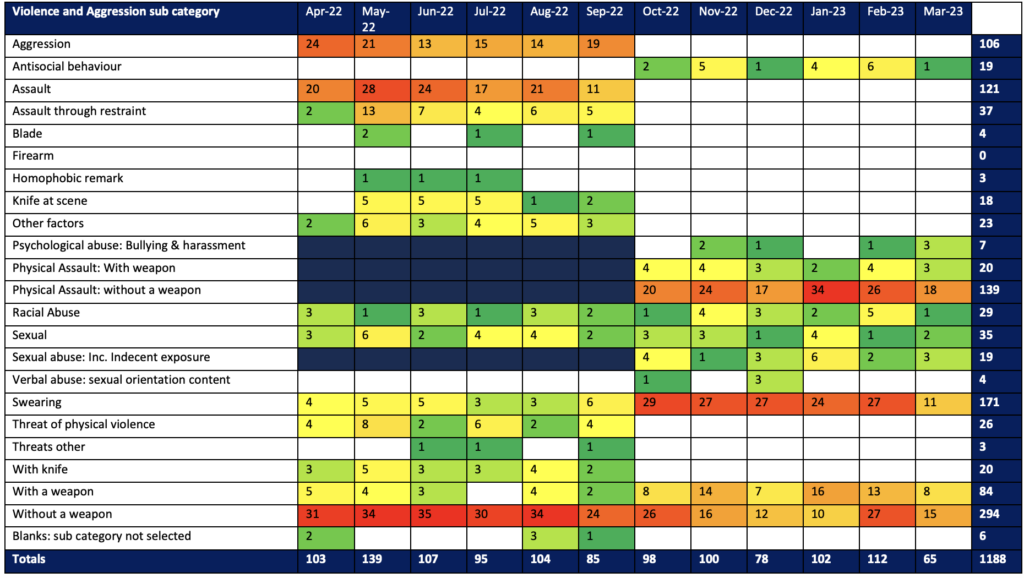
Table 28: Heat map of Violence and Aggression incidents by sub-category for 2022/23 Data source: Datix & DCIQ last accessed 18/04/2023.
7.7.5 Infection, prevention and control (IPC)
Infection, prevention and control (IPC) measures are central to protecting the health, safety and welfare of patients, service users and staff, this was particularly evident during the global pandemic. Over the last few years, guidance on emerging diseases, such as Covid-19 and Monkeypox, have been updated on a regular basis to minimise the risk of onward transmission. Our guidance is updated in line with national guidance on new variants of Covid-19 and Monkeypox and as new information becomes available. In the last 12 months there has been various changes in the government advice on testing, isolation, and vaccination of both the public and health care staff. The IPC team issued both clinical and
operational bulletins to clarify any new guidance cascaded through the operational command cells. IPC resources on the have also been updated to reflect these changes. The national infection prevention and control manual (NIPCM) principles are applied to ensure a consistent approach to IPC is maintained in the organisation. Board assurance is received through IPC sub-committee and the completion of the IPC board assurance framework (IPC BAF).
During 2022/23 we reviewed and updated the IPC Board assurance Framework focusing attention on the following ten key lines of enquiry.
IPC board assurance framework questions
- Systems are in place to manage and monitor the prevention and control of infection. These systems use risk assessments and consider the susceptibility of service users.
- and any risks posed by their environment and other service users.
- Provide and maintain a clean and appropriate environment in managed premises that facilitates the prevention and control of infections.
- Ensure appropriate antimicrobial use to optimise patient outcomes and to reduce the risk of adverse events and antimicrobial resistance.
- Provide suitable accurate information on infections to service users, their visitors and any person concerned with providing further support or nursing/medical care
in a timely fashion.
- Ensure prompt identification of people who have or are at risk of developing an
- infection so that they receive timely and appropriate treatment to reduce the risk of transmitting infection to other people.
- Systems to ensure that all care workers (including contractors and volunteers) are aware of and discharge their responsibilities in the process of preventing and
- controlling infection.
- Provide or secure adequate isolation facilities.
- Secure adequate access to laboratory support as appropriate.
- Have and adhere to policies designed for the individual’s care and provider
organisations that will help prevent and control infections.
Systems to manage and monitor infection and risks of infection
IPC guidance has been regularly updated throughout 2022/23 to ensure our guidance is in line with national guidance, particularly related to the management of nosocomial infection, testing and isolation, outbreak management and working safely. Our test, track and trace team returned to their substantive posts and the IPC team picked up the outbreak management function and contact traced staff, as necessary. Personal and environmental Covid-19 risk assessments have been reviewed and updated, as necessary. Service line assurance reports and results of IPC / hand hygiene / environmental audits are presented at the IPC sub-committee. The IPC board assurance framework is reviewed and discussed at board.
Provide and maintain a clean environment
In 2022/23 an increase in cleaning hours continued to support outbreak management. Enhanced cleaning of vehicles at emergency departments discontinued at the start of April
2022 and the IPC team worked with operations and staff side to ensure staff were aware of the change and that facilities were made available for cleaning to take place effectively.
Resources were made available to staff. Safety check points were maintained at all sites which included alcohol gel, face masks and thermometers. IPC audits continued and monthly checks were completed by operational managers. The audits were completed by IPC practitioners in line with the national IPC audit tool adapted for the ambulance service. A six weekly deep clean of all vehicles remains in place and the IPC team have introduced spot checks of these deep cleans to provide assurance.
Ensure appropriate antimicrobial use to optimise patient outcomes and to reduce the risk of adverse events and antimicrobial resistance
Although clinical staff in the organisation do not prescribe or administer large numbers of antimicrobials, mandatory reporting requirements are completed, and assurance is presented to the Clinical Effectiveness sub-committee. Clinicians follow the Paramedic Drug Formulary for Antibiotics and JRCALC Guidance for Benzylpenicillin.
Provide suitable information on infections for staff and patients
Action cards were updated for crews managing infectious patients in line with national guidance within vehicles and to support ventilation within vehicles. National guidance and local operating processes disseminated regularly to staff via bulletins, social media, internal intranet, and the IPC cell. All training materials for staff and volunteers was reviewed. IPC infographics/posters displayed in the back of ambulances.
Identification of people at risk of developing an infection and onward transmission
Asymptomatic testing of health care staff was ceased in line with national guidance this year, testing kits continued to be available on the government portal for symptomatic staff. We had some supplies of kits that had been distributed earlier in the pandemic – during an increase in outbreaks at the call centres these kits were distributed to these centres so any
staff who developed symptoms during their shift could be tested, and appropriate action taken.
Prevention of onward transmission of infection was the focus by ensuring that infection control measures were being adhered to – these measures included: protective screens and barriers across call centres, reduced occupancy of offices and home working where appropriate, individual and environmental risk assessments. Measures such as social distancing and universal mask wearing were stood down with the caveat that if prevalence of Covid-19 increased the measures would be implemented once again. These control measures were implemented in partnership with trade union colleagues and in line with national working safely guidance.
A review of the PTS booking process to place to ensure that there was a robust risk assessment of patients that required transportation.
Systems to ensure staff discharge their responsibilities for IPC
Regular bulletins and guidance were regularly published for staff and available on the intranet – these were published as any national guidance had been updated.
All IPC policies have been reviewed, updated and approved by the IPC sub-committee and are available to our staff, IPC training packages and posters were updated and available for use by all staff. Short educational videos for staff have been developed and distributed.
Fit testing procedures were updated following a scoping exercise on compliance in the summer of 2022. Ashfield Health was brought in to support with fit testing and to improve compliance rates across the organisation from September 2022. All staff who fit the required criteria have been provided with respiratory protective equipment hoods. All fit testing is recorded centrally on ESR making it easier to identify compliance rates and ensure that all staff now have a central record of which masks they have been fit tested to. This updated process and recorded has been monitored by the Respiratory Protective Equipment group which was formed in September 2022.
- Medicines management
We are committed to high quality medicines optimisation within the service through having the right medicines available, having the right governance to support medicines use, ensuring medicines are available for use, ensuring medicines are of a suitable quality and supporting medicines to be used safely.
The following areas provide the workplan for the work undertaken by the Medicines team during 2022/23:
Clinical effectiveness of medicines:
- Implementation of changes to our medicines formulary, including widening access to naloxone administration to treat opiate overdoses and introducing an antibiotic to minimise infection in patients with an open fracture.
- Clinical induction medicines management training has been updated, three new e- learning packages have been developed (naloxone, DuoDote and co-amoxiclav), update sessions on medicines to the MERIT team have been delivered and training of undergraduate paramedics continues.
- Clinical guidance on administration of adrenaline for post cardiac arrest patients with a return of systemic circulation has been updated alongside the training.
- Methoxyflurane has been approved for doctor use in the North West Air Ambulance and calcium chloride injection has been approved to support North West Air Ambulance paramedics to administer blood products.
- Clinical approval for additional pain relief options has been received and an implementation plan is being worked on.
Robust governance for medicines use:
- All PGDs required are in place and in date.
- A new PGD for co-amoxiclav was implemented and all staff trained.
- A review of influenza vaccine handling was carried out.
- An audit of ketamine use has been carried out.
- A thorough review of the Medicines policy has been completed.
- All medicines procedures have been reviewed and updated.
Safe and secure handling of medicines:
- Securing funding to expand the footprint of the medicines supply hub. This brings many benefits including that it will allow a dedicated goods in and goods out flow.
- Reengineering of processes for nerve agent countermeasure medicines. They are now all supplied from the medicines supply hub (in line with how other medicines are supplied), in the same distinctive pouch that is tamper evident, stored in a standardised place on ambulances and recorded on the SafeCheck system for visibility.
- Strengthening controlled drug handling arrangements with a focused group to oversee all aspects of governance and a new dashboard to monitor usage.
- A successful Home Office inspection has been achieved and a review of estate security around medicines is underway during 2023.
Medicines safety:
- Learning lessons bulletin published.
- Medicines safety campaign delivered tied in with World Patient Safety Day focused on right dose, right route adrenaline 1 in 1,000 injection.
- Improved safety and governance of medicines used for patients as part of end-of-life care.
- Review of the Patient Safety Alert ‘Use of oxygen cylinders where patients do not have access to medical gas pipeline systems and risk assessment conducted and actions completed.
- Set up or an End-of-Life Care Working Group which has reviewed handling of medicines and developed communications to support clarity around medicines administration.
- A workstream has been focusing on medicines preparation and administration, this has resulted in a variety of tools being developed and implemented.
- Care Quality Commission
As of 31 March 2023, our overall CQC ratings remain the same as the 2020/2021 Quality Account:
| Ratings | |
| NWAS overall rating | Good |
| Are services safe? | Good |
| Are services effective? | Good |
| Are services caring? | Good |
| Are services responsive? | Good |
| Are services well-led? | Good |
Our overall CQC Inspection ratings matrix is as follows:
| Safe | Effective | Caring | Responsive | Well-led | Overall | |
| U&EC | Good | Good | Good | Outstanding | Good | Good |
| PTS | Good | Good | Good | Good | Requires Improvem ent | Good |
| EOC | Good | Good | Good | Good | Good | Good |
| Resilience | Good | Good | Not rated | Good | Good | Good |
| NHS 111 | Good | Good | Good | Good | Good | Good |
| Overall | Good | Good | Good | Good | Good | Good |
In 2022/2023 the CQC continued to regulate providers using a risk-based model whilst moving towards their new regulatory model, which commences in April 2023. Their approach during 2022/23 included several non-rated inspections in Urgent and Emergency Care services and 111 and ongoing routine engagement meetings and enquiries.
In February 2022 the CQC announced a system level focussed inspection of Urgent and Emergency care within the Lancashire and South Cumbria Integrated Care System (ICS) and each of the partner agencies within the ICS, and a similar a similar inspection in North Mersey. The CQC also inspected our NHS 111 service.
Inspection reports were received for paramedic emergency service within the geographical footprints, the emergency operational control service and 111, with system summary reports for the two ICBs also being received for review. We provided feedback and comment on the system summary reports in line with CQC required timescales. The inspections were not rated and thus the overall ratings for us remained the same, with ‘Good’ overall.
Overall, the inspections provided strong recognition of the safety and quality of our services and no enforcement action was required. Furthermore, no follow up inspection for the organisation was tabled. Several best practices were noted in within the ‘innovation
station’ at Kendal, that there was a strong focus on continuous improvement throughout
and that we controlled infection well.
Six ‘should do’ actions were suggested for PES and EOC. These were to:
- Continues to take appropriate actions to improve ambulance response times in line with nationally agreed targets. (UEC)
- Continue to influence and play a key role in the increasing demand on urgent and emergency care capacity, patient harm, and unmet patient needs throughout urgent and emergency care along with system partners and others. This should include a focus on improving the safety and effectiveness of services for patients and of its frontline and support staff. (UEC)
- Develop clearer guidance for staff for the cleaning frequency of ambulance vehicles. (UEC)
- Continue to proactively monitor call demand to ensure staffing levels are appropriate. (111)
- Continue to review call audit data to meet the required national targets. (111)
- Continue with plan of safeguarding training for all clinicians. (111)
7.9 Quality assurance visits (QAV)
We conducted annual quality assurance visits (QAVs) across PES, PTS, HART, and contact centres since 2012. The purpose of QAVs is to provide assurance about the quality and safety of operational premises, vehicles and services at sector level and provide internal second line assurance and information in relation to key lines of enquiry from the Care Quality Commission.
QAVs include several health and safety focused assessments in parallel to other audits such as the Health and Safety Workplace Inspection, Fire Risk Assessment, Infection, Prevention and Control Audits.
After the QAV takes place, the nominated QAV lead produces a report comprising a summary of the key findings and an action log, which is then submitted to the Head of Operations for sign off. This includes an internal rating system that scores each area assessed as outstanding, good or requires support.
A central repository of all QAV reports and actions is held on our knowledge management system, SharePoint. The overall position for QAV compliance (as at 27/03/2023) is strong with 94% of all operational sites having received a QAV in the last 12 months.
Each sector has their own integrated action tracker, which is stored on an Excel spreadsheet, in our knowledge management system, SharePoint. The integrated action trackers are managed locally by area administrators and contain actions from various audits. As of 27 March 2023, the current action completion position was challenging with each area averaging at over 70% compliance for closure of actions.
Following imminent changes to the CQC’s regulatory model (single assessment framework), we have commenced the journey to redesign our internal QAV assessment framework. This will ensure our internal assurance systems are aligned to CQC’s new Quality Statements
which have replaced the key lines of enquiry and prompts. This is also an opportunity for us to redesign our internal assurance processes to further improve oversight of safety.
7.10 Skills and training
For 2022/23 mandatory training focus was maintained on statutory/high risk minimum content, with the primary impact that the PES classroom training was reduced to one day instead of two days, to manage the statutory/risk minimum and reduce risk of cancellation of whole programme should system pressure necessitate the reset of staff abstractions. On- line learning modules remained the same. All areas have met or exceeded their compliance targets with the overall year-end position of 88% compliance against a target of 85%.
The third and final module (Follow Up) from the national Freedom to Speak Up suite of learning was released and mandated for all senior leaders.
Within our leadership development programme, the Beyond Bias module commenced delivery and this is mandated for all leaders with people management responsibilities. Delivery of this programme will cross financial years.
7.11 Equality, diversity and inclusion
Promoting and supporting diversity in the workplace contributes towards employee wellbeing and engagement and a diverse workforce can drive an organisation’s effectiveness through enabling people to reach their full potential, in turn improving innovation and decision-making, as well as meeting the needs of a diverse population.
We continue to work with partners across the region and nationally in collaboration on activities and to share best practice about inclusion. We work proactively to be visible as an employer of choice across all our communities. We strive to reduce the health inequalities faced by our most vulnerable patients across the North West.
We are committed to creating a culture of openness and transparency. As a requirement of the Public Sector Equality Duty, we must capture a range of equality related information and report on it and a statutory obligation under the Equality Act 2010 to publish a range of monitoring information relating to workforce, patients and the local community. This data and narrative include the Workforce Race Equality Standard (WRES), Workforce Disability Equality Standard (WDES), Equality Delivery System (EDS), Gender Pay Gap Reporting and the Public Sector Equality Duties (PSED).
During 2022/23 a priority has been to embed equality, diversity and inclusions (EDI) across our services and work programmes. Work to date includes:
Overhaul of the current equality impact assessments in recognition of the need to increase the confidence how to use and interpret the results to support decision making from the start of any work/project and taking views from wider stakeholders.
Embedding staff networks (LGBT+, race equality, disability, armed forces and gender) to encourage involvement in quality programmes of work and to strengthen visibility, advocacy and intersectionality.
Established systems for the measurement, monitoring and reduction of inequalities within programmes and across quality service lines using NHS staff survey, National Quarterly Staff Survey (NQPS), WRES, WDES, gender pay gap reporting to sustain and maintain representation.
A specific focus on recruitment and engagement opportunities to create a more diverse and representative workforce.
Engagement of an external consultant to undertake a Recruitment Audit to focus on offering a deep dive into the end-to-end process exploring the experiences of applicants and hiring personnel as they navigate each stage. The audit will prioritise accessibility and inclusion for all and will consider barriers to recruitment and attraction too all minority groups with a specific focus on those from BAME Backgrounds.
Design and Delivery of the Beyond Bias programme aimed at leaders.
Commencement of the reverse mentoring programme.
Focus on the opportunities for career progression and consideration of any barriers which may prevent progression of staff across protected groups.
Ensuring recruitment, training and development opportunities are fair, open and transparent to all, supported by diverse panel members i.e., gender split and working with the learning and organisational development manager with a focus on EDI.
7.12 Right Care Strategy refresh
The Quality strategy development process includes four phases: diagnose, design, develop, and evaluate. The strategy is currently in the development phase, extensive diagnosis work has been undertaken to analyse the current context and to engage staff and patients to understand their experiences and outcomes and this engagement has been used to design a strategy which will align to our strategy’s aim to provide high-quality, inclusive care.
Whilst the new Quality strategy is in development, we have continued to align plans to provide care which is safe, effective and person centred.
8. Looking forward to improving care
- 2022/23 Priority areas for improvement Safety
- To embed a safety and learning culture into the organisation via the implementation of the Patient Safety Incident Response Framework.
- To develop learning mechanisms which allow patient safety insights to be generated from a range of data.
- Training needs analysis to identify key roles for advanced safety training and design structured leadership training.
- To work collegiately with the North West regional maternity team to review and align services where applicable to the single maternity plan via NHS England.
- To create increased parity of response for individuals calling 999/111 in mental health crisis. We will help to achieve this by having a robust model of trained mental health practitioners in call centres, and by implementing mental health response vehicles across ICB footprints.
- To deliver IPC standards by embedding the National Standards of Cleanliness for contact centres and vehicles.
- To ensure there is a reliable IPC dashboard which provides real time data.
- To ensure there is a reliable data source for reporting safeguarding through Cleric and reviewing the needs of the organisation in relation to safeguarding training.
- To embed a safety and learning culture into the organisation via the implementation of the Patient Safety Incident Response Framework.
Effectiveness
- All nationally mandated clinical data collections for the 999 service are completed on time in full each month and the new national audits are implemented e.g., Falls.
- To deliver ePR phase 2 e.g., enabling the use of the Directory of Service within ePR to allow patients to be referred to the right place of treatment.
- To reduce variation in clinical practice, focusing on see and treat.
- To develop new safe pathways of care and processes through clinical audit, handover and improve response times.
Patient Centred
- To enable access to patient’s records via ePR.
Quality compliance
- To ensure we maintain a ‘Good’ CQC rating.
- To ensure we can deliver safe systems of work for staff in line with Health Safety Executive regulatory standards.
- To strengthen internal quality assurance through the review of existing processes and in line with the new CQC framework which goes live in April 2023.
Equality, diversity and inclusion
- To begin implementation of the learning disability and autism strategic plan and improve outcomes for high risk/vulnerable patient groups.
9. Formal statements on quality
9.1 Review of services
We reviewed all the data available on the quality of care in the services provided by us in 2022/23. The income generated by the NHS services reviewed in 2022/23 represents 100% of the total income generated from the provision of NHS services by the trust.
9.2 Participation in clinical audits
NHS England Ambulance Quality Outcome Indicators
English ambulance services are required to undertake specific ambulance clinical audit and submit the data, according to a prefixed schedule, directly to NHS England. The ambulance service clinical audit data also informs the out-of-hospital cardiac arrest registry, Senitnal Stroke national audit project and the Myocardial Infarction national audit project.
The list of mandated audits is:
Outcome from cardiac arrest – return of spontaneous circulation (ROSC):
- Overall
- Utstein comparator group
Outcome from cardiac arrest – survival to discharge:
- Overall
- Utstein comparator group Post ROSC Care Bundle:
- The number of patients who received the appropriate care bundle after sustaining ROSC for 10 minutes or longer after an out-of-hospital cardiac arrest where resuscitation (advanced or basic life support) was commenced/continued by ambulance service.
Outcome from acute ST-elevation myocardial infarction (STEMI):
- Time from call to angiography.
- The number of patients with a pre-hospital diagnosis of suspected ST elevation myocardial infarction confirmed on ECG who received the appropriate care bundle.
Outcome from stroke:
- Time from call to hospital arrival.
- The number of Face Arm Speech Test (FAST)- positive or suspected stroke patients assessed face-to-face who received the stroke diagnostic bundle.
- Outcome from sepsis: Audit retired during 2022/23.
- The number of patients with suspected sepsis with a NEWS of 7 or above assessed face-to-face who received an appropriate care bundle.
This data is published nationally: https://www.england.nhs.uk/statistics/statistical-work- areas/ambulance-quality-indicators/
As anticipated the outcome from sepsis measure has been retired and replaced by a pilot measure reviewing the care received by patients who are over 65 years, have fallen from a standing height or less and discharged at scene. Patients falling accounts for 10-25% of emergency ambulance responses each year. The rationale for the new audit is driven through falls association with increased morbidity and mortality, therefore having an impact on quality of life, health, and healthcare costs. It is important to assess the practice and behaviour that our ambulance clinicians provide to this patient cohort when discharging at scene.
The falls dataset was approved mid-year and scheduled to replace the sepsis submissions due in December 2022 and repeated on a quarterly cycle. Through negotiation with NHS England the submission schedule was postponed enabling ambulance trusts to develop mechanisms to undertake the new audit. The first data submission will be in June 2023.
9.3 Participation in clinical research
North West Ambulance Service provides high quality care to our patients by meeting not only their immediate healthcare needs, but also having a positive impact on their future
health and wellbeing. As an NHS organisation, we have a responsibility to provide our patients, staff and the public with the opportunity to participate in health care research.
Our Research strategy expresses our commitment to host and develop research that will not only enhance the quality of the urgent and emergency care we deliver but will ensure that the communities we serve have equitable access to our high quality, clinical services to continue improving the health outcomes for all our patients.
Our mission is to embed a culture of research excellence and to be at the vanguard of generating new evidence that supports the delivery of first-rate, urgent and emergency care.
Our vision is to enhance the health and wellbeing of the communities we serve by translating high quality research into exceptional service provision and outstanding clinical practice.
The Medical Directorate is accountable for research. Under the direction of our consultant paramedic in their role of research lead, we have continued to make strides in embedding research across our organisation.
Income secured from the National Institute for Health and Care Research (NIHR) supports
2.0 whole time equivalent NIHR Research Paramedics. Our research paramedics promote and deliver NIHR research across the organisation, ensuring that patients, staff and the public can take part in research.
For the third consecutive year, the trust successfully triggered NIHR Research Capability Funding (RCF) by successfully recruiting participants to NIHR Clinical Research Network (CRN) Portfolio research studies. The purpose of NIHR RCF is to help research-active NHS organisations to act flexibly and strategically to maintain research capacity and capability.
Our staff were principal investigators and local collaborators for NIHR CRN Portfolio studies, and we continued to offer researcher development opportunities. Staff undertook a Data Science Research Internship with NIHR Applied Research Collaboration (ARC) North West Coast and were part of the NHS R&D North West and NIHR North West Research Workforce Learning and Development North West Early Career Researcher Development Pathway
programme. We hosted a Bitesize Research seminar in collaboration with NIHR CRNs Greater Manchester and North West Coast to apprise staff of research taking place at the trust and inform them about how they can get involved in supporting research.
Our consultant midwife was appointed as an NIHR senior research leader for nursing and midwifery programme positions. The programme aids to establish researchers to help lead initiatives to promote a research active culture through empowering other nurses and midwives to support, lead and deliver research.
We actively maintained partnerships with our local NIHR Applied Research Collaborations (ARCS) and CRNs, through which we engage with health and care providers, academia and other external stakeholders to cultivate research collaborations. The team won the ‘Collaborative Working Accomplishment’ at the NIHR CRN Greater Manchester Health and Care Research Awards 2022 for an end-of-life advance care planning project devised and delivered with NHS and academic partners in the North West.
We remained an active member of the National Ambulance Research Steering Group (NARSG) through which we access opportunities to be involved in grant applications and upcoming research studies, enhancing our reputation as a research-active organisation.
We publicised research opportunities, successes and achievements both internally and externally through regular communications bulletins, social media and via dedicated pages on the website and intranet. With our staff app that allows for subscribers to be notified of new research studies that staff can be involved in delivering or participating in.
9.3.1 Performance in clinical research
In 2022/23, we opened 12 new research studies that were approved by the NHS Health Research Authority (HRA). 7 of the newly approved research studies were NIHR CRN Portfolio studies. 913 research participants including staff, patients and the public participated in all NIHR CRN Portfolio research studies that were open to recruitment in this fiscal year, see table below.
| Clinical Research Network Portfolio Performance | ||||
| Financial Year | 2019-20 | 2020-21 | 2021-22 | 2022-23 |
| Number of Studies Approved | 7 | 6 | 11 | 7 |
| Participants Recruited to OpenStudies | 645 | 606 | 625 | 913 |
During 2022/23, confirmation of capacity and capability was issued for 7 NIHR CRN Portfolio studies:
- Developing palliative and end-of-life care research partnerships and capacity in the North West Coast of England.
- Identifying the impact of a colleague’s suicide on NHS staff, and their support needs,
to inform postvention guidance.
- Ambulance clinician approach to acute head injuries in older adults: A mixed- methods study in clinical decision-making.
- Co-producing an Ambulance Trust national fatigue risk management system for improved Staff and Patient Safety (CATNAPS).
- Paramedic decision making during out of hospital cardiAC arresT 2. A mixed- methods study (The REACT2 Study).
- Hypo-RESOLVE: Developing a preference-based quality of life (QoL) measure to determine the impact of hypoglycaemia in people with diabetes.
- Behavioural Activation for Low mood and anxiety in Male NHS frontline workers: The BALM programme.
In 2022-23, confirmation of capacity and capability was issued for 5 non-Portfolio studies:
- A mixed-methods study to evaluate current practice and explore current challenges relating to the triage of patients with a head injury in the pre-hospital environment.
- The relationship between emotional intelligence, self-compassion and wellbeing in ambulance staff.
- Improving the Experiences of Black African Caribbean Men Detained Under the Mental Health Act: A Co-Produced Intervention Using the Silences Framework (IMPROVE- ACT)
- The Psychology of Interoperability: Critical Decision Method Interviews.
- Head injury Evaluation and Ambulance Diagnosis to avoid Hospital emergency admission: a HEAD HOME feasibility study.
9.3.2 Research grants
We were a co-applicant for a successful NIHR Health Technology Assessment Application Acceleration Award for the ‘Randomised evaluation of clinical Outcomes using novel Technologies to optimise antimicrobial Therapy (PROTECT)’ project.
9.3.3 Research publications
The following research publications were either authored or co-authored by staff at North West Ambulance Service NHS Trust in the financial year 2022/23:
- Alqurashi, N., Alotaibi, A., Bell, S., Lecky, F., & Body, R. (2022). The diagnostic accuracy of prehospital triage tools in identifying patients with traumatic brain injury: A systematic review. Injury [online], 53(6), pp. 2060-2068. Available at https://doi.org/10.12968/jpar.2022.14.9.CPD1
- Alqurashi, N., Alotaibi, A., Bell, S., Lecky, F. and Body, R. (2023). Towards exploring current challenges and future opportunities relating to the prehospital triage of patients with traumatic brain injury: a mixed-methods study protocol. BMJ Open [online], 13(3), e068555. Available at: https://doi.org/10.1136/bmjopen-2022- 068555
- Bell, S., & Hill, J. E. (2022). Prehospital triage tools in major trauma: a critical appraisal of a systematic review [CPD: Major Trauma]. Journal of Paramedic Practice [online], 14(9), pp. 1-4. Available at https://doi.org/10.12968/jpar.2022.14.9.CPD1
- Bell, S., Pennington, E., Hill, J., & Harrison, J. (2022). Prehospital airway management [Commentary]. Journal of Paramedic Practice [online], 14(2), pp. 51-53. Available at: https://doi.org/10.12968/jpar.2022.14.2.51
- Heys, S., Rhind, S., Tunn, J., Shethwood, K., & Henry, J. (2022). An exploration of maternity and newborn exposure, training and education among staff working within the North West Ambulance Service. British paramedic journal [online], 7(2),
- pp. 50-57. Available at: https://doi.org/10.29045/14784726.2022.09.7.2.50
- McElroy, L., Robinson, L., Battle, C., Laidlaw, L., Teager, A., de Bernard, L., McGillivray, J., Tsang, K., Bell, S., Leech, C., Marsden, M., Carden, R., Challen, K., Peck, G., Hancorn, K., Davenport, R., Brohi, K., & Wilson, M. S. J. (2022). Use of a modified Delphi process to develop research priorities in major trauma. European journal of trauma and emergency surgery: official publication of the European Trauma Society [online], 48(2), pp. 1453-1461. Available at: https://doi.org/10.1007/s00068-021-01722-z
- Pennington, E., Bell, S., Wright, A., & Hill, J. (2023). Impact of COVID-19 on out-of- hospital cardiac arrest care. Journal of Paramedic Practice [online], 15(2), pp. 74-77. Available at: https://doi.org/10.12968/jpar.2023.15.2.74
- Pennington, E., Price, J., Bell, S., & Hill, J. (2022). Prevalence, severity and preventability of prehospital patient safety incidents. Journal of Paramedic Practice [online], 14(7), pp. 298-300. Available at: https://doi.org/10.12968/jpar.2022.14.7.298
- Thoburn, S., Cremin, S., & Holland, M. (2022). An atypical presentation of orthostatic hypotension and falls in an older adult. British paramedic journal [online], 6(4), pp. 41-47. Available at: https://doi.org/10.29045/14784726.2022.03.6.4.41`
- Thomson, G., Balaam, M.-C., Nowland Harris, R., Crossland, N., Moncrieff, G., Heys, S., Sarian, A., Cull, J., Topalidou, A., & Downe, S. (2022). Companionship for women/birthing people using antenatal and intrapartum care in England during COVID-19: a mixed-methods analysis of national and organisational responses and perspectives. BMJ open [online], 12(1), e051965. Available at: https://doi.org/10.1136/bmjopen-2021-051965
- Wilson, C., Howell, A.-M., Janes, G., & Benn, J. (2022). The role of feedback in emergency ambulance services: a qualitative interview study. BMC Health Services
- Research [online], 22(296), pp. 1-11. Available at: https://doi.org/10.1186/s12913- 022-07676-1
9.4 Use of the CQUIN payment framework
This year the flu programme was aligned with one of the quality indicators in the 2022/23 Commissioning for Quality and Innovation (CQUIN) with a goal of vaccinating between 70% to 90% of frontline staff. This funding was provided at the start of the campaign and was not linked to any financial penalty in the event the targeted vaccination rate was not met. The frontline vaccinated figure for our service at the end of the campaign reported was 49% and we sat well within the average rate of vaccinations when compared to other trusts of a similar size across the region. A reduced uptake of the flu vaccine was reported across the wider NHS with the main reason being vaccine fatigue cited for this year’s decline in uptake.
10. Statement on relevance of data quality and improvements
Please find the North West Ambulance Service NHS Trust statements on data quality.
- NHS Number and General Medical Practice Code Validity
North West Ambulance Service NHS Trust did not submit records during 2022/23 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. This requirement did not apply to ambulance trusts during 2022/23.
- Clinical coding error rate
North West Ambulance Service NHS Trust was not subject to the Payment by Results clinical coding audit during 2022/23 by the Audit Commission.
- Data Security and Protection Toolkit (DSPT) attainment levels
North West Ambulance Service NHS Trust DSPT baseline submission assessment provided an overall score for 2022/23 was 93.8% (106 of the 113 compliance standards were met) with a published status of ‘approaching standards when it was submitted in February 2023. Actions have since been taken to address the outstanding assertions and the trust now meets 99% (112 of the 113 standards). The final DSPT submission is due 30th June 2023, and the only outstanding requirements is for 95% of staff to have completed Data Security Awareness training. An improvement plan for how to achieve 95% of staff having completed the Data Security Awareness training will be developed alongside the Learning and Development team.
11. Integrated care board, Healthwatch and health scrutiny committee statements
ICB Statement in response to the NWAS Quality Account 2022/23
Introduction
Lancashire and South Cumbria Integrated Care Board (ICB) undertakes the role of Lead Commissioner for Ambulance and NHS 111 Services on behalf of ICBs that make up the North West region. In doing this it ensures that robust Commissioning, Quality, Contract and Performance Management is in place to enable and support North West Ambulance Service (NWAS) to provide effective services to the circa 7.5 million residents of the North West.
These services comprise:
- Paramedic Emergency Service: the 999 ambulance service
- NHS 111 services
- Patient Transport Services: enabling eligible patients to access outpatient, discharge and other hospital appointments for Greater Manchester, Merseyside, Lancashire and Cumbria. Services for Cheshire are not provided by NWAS.
In its role as Lead Commissioner, Lancashire and South Cumbria welcomes the opportunity to review and support the 2022/23 NWAS Quality Account and this statement is made on behalf of the North West Ambulance Strategic Partnership and Transformation Board (SPTB) representing the North West ICBs.
To the best of our knowledge the information presented in the Quality Account accurately reflects the work undertaken by NWAS in 2022/23 to improve the quality of the services it provides. Lead Commissioners would like to acknowledge the extremely challenging period 2022/23 was for the whole of the NHS, and the work undertaken to support the population of the North West during this period by NWAS.
Ambulance and NHS 111 services governance
NWAS provides services across five “county” areas; North Cumbria; Lancashire and South Cumbria; Cheshire, Warrington and Wirral, Merseyside and Greater Manchester. This is a complex geography where the “county” footprints now form 3 full ICB footprints of Lancashire and South Cumbria, Greater Manchester and Cheshire and Mersey, North Cumbria as part of North East and North Cumbria and Glossop as part of Derby and Derbyshire.
The Ambulance Commissioning Team (hosted by Lancashire and South Cumbria) is funded by the 5 ICBs and operates under a Memorandum of Understanding (MOU) signed by all ICBs. The MOU allows the team on behalf of the North West ICBs to commission ambulance and NHS111 services in the region serviced by NWAS. Co-ordination of contract agreement and management is through an extensive governance structure.
The Strategic Partnership Transformation Board (SPTB) operates on behalf of the 5 ICBs and is attended by a designated ICB lead at executive level as well as by Senior Clinical Leads from each area. The primary function of the SPTB is to assure commissioners that NWAS are meeting all required national targets and KPIs and deliver safe and effective services.
To support this there are several formal sub-groups in place ensuring effective coordination and management of the contracts held with NWAS. These are:
- Regional Clinical Quality Assurance Committee (RCQAC); comprising the Regional and nominated County Clinical Leads with other clinicians, the Lead Commissioning Team and NWAS. Responsible for reviewing and assuring serious incidents where harm has arisen from operational process, clinical decision-making or care delivery, clinical audit and oversight of clinical changes to services. Each county has its own local meeting to review incidents and clinical safety linked into the RCQAC governance process.
- Quality & Safety Group (Q&S); a multi-disciplinary group of nominated county qualified representatives, lead commissioners and NWAS, including clinical oversight. Reviewing and assuring, workforce, safeguarding, Health and Safety, patient experience and the introduction of the Patient Safety Incident Response Framework (PSIRF).
- Operational Delivery Group (ODG); is a collaborative meeting with NWAS, lead commissioners, ICB Leads and NHS England to develop the years Key Priorities and create a work plan to deliver improvements in performance and service developments.
- The governance arrangements are reviewed annually and are aligned to the National Commissioning Framework for Ambulance Commissioning.
2022/23 quality account overview
Paramedic Emergency Services (PES)
Commissioners recognise that NWAS, along with many NHS providers and systems, has faced significant challenges in 2022/23, especially during the winter period. This, along with most English ambulance services, has resulted in patients waiting at times longer than would be hoped for an ambulance. Due to local pressures many then experienced further delays at times to be handed over to hospital staff. Sadly, at times this has also contributed to patient harm and poorer outcomes.
At the start of 2022/23 many NHS services were still feeling the effects of Covid-19 and trying to recover their position to pre Covid-19 levels, whilst reducing waiting lists that had lengthened during the pandemic. Although the overall number of incidents and 999 calls did reduce in 2022/23 in comparison to 2021/22 system pressures and industrial action later in the year did impact on NWAS, with high media attention on delayed hospital handovers and longer response times. To aid this situation NWAS utilised private ambulance services, volunteers and voluntary services and employed more 999 call takers with extra funding provided by commissioners and released by NHS England to assist with the pressures felt.
NWAS also trained military staff and utilised Military Aid to Civil Authorities (MACA) between December and March to aid improving response times for patients. Work was also
undertaken by the Operational Delivery Group (ODG) to improve response times through key priorities of work being identified, and their progress monitored monthly.
Commissioners have also worked closely with the trust and ICB leads to improve response times and to support alternative pathways of care for those patients that can be supported by alternative services, rather than being transported to A&E. During the winter period Amanda Pritchard from NHS England requested assistance from ICBs for ambulance services to respond to patients that had fallen, were unable to get off the floor unaided, had no life- threatening injuries or illness and had called 999. This was to free ambulance crews to respond to more life-threatening calls. This resulted in lead commissioners, NHS England and ICBs working collaboratively with NWAS to gain access to lifting services across the North West to respond to uninjured fallers still on the floor calling 999. NWAS had already developed a system in Lancashire and South Cumbria which was adopted by the other ICBs and allowed NWAS to alert these local services to the incident. These local services are now able to respond in a timely manner, assist these patients off the floor, and then link patients back into local community services or NWAS to further support patients where appropriate for ongoing care. It was pleasing to see such a driven and fast-moving collaborative piece of work with the majority of the North West covered by January 2023. This pathway of care was also opened up further with local 2-hour Urgent Community Response services responding to fallers with minor injuries and illness who had called 999.
After a very challenging December and January it is pleasing to see a reduction in response times at the end of 2022/23, indicating the positive impact the collaborative work to improve hospital handovers across the region and improve alternative pathways of care is having. This work will continue into 2023/24 as NWAS aim to achieve Ambulance Response Programme targets, and better support the population of the North West, via ODG.
The introduction of NHS Pathways as the primary triage system for 999, to assist in aligning the call centres in NWAS with 111 to create integrated contact centres, was also positively received. This significantly increased hear and treat, where NWAS could identify patients at the initial call that did not need an emergency response and signpost/refer into more appropriate services for their need. This in turn released emergency ambulances to respond to more life-threatening calls. This consistency of offer by NWAS for their patients and
identifying appropriate pathways of care sooner in the patient’s journey can only have better outcomes for the North West population, and the whole NHS system. It also allows for greater resilience in the workforce and further opportunities for NWAS staff.
NHS 111
This was also a challenging period for NHS111, with Covid-19 and the Strep A outbreak increasing demand at times. It was pleasing to see overall the number of 111 calls offered reduced on the previous year and the number of calls answered in 60 seconds increasing from 18.65% to 36.85%. In total NHS 111 answered almost 1,750,000 calls for the North West.
During the pandemic NHS 111 has had a significant shift in their activity. Pre Covid-19 111 was predominantly an access to the out of hours service, with many staff working nights and weekend, whilst during Covid-19 there was an increase in day time calls to assist in accessing the right care for people 24/7. This has led to many challenges with workforce and fulfilling roster requirements that fit 111 demands, and as Covid-19 restrictions lessened staff reverting to previous careers held before Covid-19. NHS 111 has worked with lead commissioners and NHS England on how retaining and recruiting staff can be achieved. The introduction of NHS Pathways as the primary triage for 999 will now give greater flexibility to the 111 workforce for their development across the 2 service lines, which is hoped to retain staff.
Several initiatives over the year have been introduced with the utilisation of SMS texting for care advice, with advice being sent via text where the patients IT is appropriate. This not only frees Health Advisors to deal with the next waiting call but gives the patients written confirmation of the advice given they can then refer back to if required. It is also encouraging to see the introduction of Learning Forums to support staff and share learning but also how it is developing improved new ways of working, including the introduction of digital alerts.
The introduction of Visual Interactive Voice Response (VIVR) is also good to see, with patients able to (where the technology allows) input their own demographics onto the
system, allowing the call taking to concentrate on the patient’s current concern/presentation and reducing call handling times.
Patient Transport Services (PTS)
PTS was significantly impacted by the pandemic with initially many transportation requirements cancelled as hospital appointments were cancelled. With a reduction in activity PTS released its staff to support PES operations as their performance became more challenging. Once appointments re-started in hospital the IPC requirements for patient transportation resulted in reduced capabilities of transport with social distancing still being in place.
It has been pleasing to see in 2022, as the Covid-19 restrictions were lifted regarding transporting patient in vehicles with multioccupancy by NHS England, to see an increase of activity to 85% pre Covid-19 levels, especially as some appointments have continued to be over the telephone therefore not requiring PTS transportation.
PTS did assist NHS systems over the pressured winter period by assisting in a more responsive discharge service, therefore assisting the NHS economy in releasing beds for waiting patients. The PTS bureau assisted demand over the industrial action periods, with some of their staff trained in 999 call taking. Both of these need acknowledging and thanks.
Patient safety
Not surprisingly during such a pressured period NWAS, along with many NHS services, has seen complaints and concerns regarding delays as one of the main themes across all service lines. Delays for Paramedic Emergency Service can have a more profound impact on patients than other services and PES has seen an increase in serious incidents involving delayed response in 2022/23 in comparison to previous years, as have most ambulance services. Commissioners would like to acknowledge the work undertaken by NWAS to investigate these difficult incidents, whilst also involving external stakeholders in the investigation at times, which has historically been challenging. With the work undertaken by NWAS so far with the implementation of PSIRF it is hoped when things do go wrong the new processes of PSIRF will make investigations easier for families with greater input from them
and will support improvement more effectively to prevent future harm occurring. Currently serious incidents are reviewed at the Regional Clinical Quality Assurance Committee (RCQAC), chaired by the lead commissioners, where these incidents are tied into the work being undertaken by ODG to improve response times and give better patient outcomes in the future. RCQAC also ensures that all possible lessons learnt from any serious incidents are identified, to again prevent potential future harm occurring.
The increased inclusion by NWAS of patients and their families with new Patients Safety Partners and the NWAS Patient Public Panel is welcomed, as is the increase in profile of patient safety which all aligns with the NHS Patient Safety Strategy and the transition to PSIRF in 2023/24.
Care Quality Commission
NWAS was included in some of the new system level focussed CQC inspections of urgent and emergency care within the Lancashire and South Cumbria Integrated Care System (ICS) and each of the partner agencies within the ICS, as well as a similar inspection in North Mersey. PES and the Emergency Operations Centre were included if in their locality. It was re-assuring that the inspections provided recognition of the safety and quality of NWAS services, and no enforcement action was required. 111 did receive its own inspection. These inspections have not changed NWAS overall CQC rating which remains Good, with 6 ‘should do’ actions including:
- Take appropriate action to reduce response times for PES.
- A focus on improving the safety and effectiveness of services for patients and of its frontline and support staff for PES.
- Develop clearer guidance on cleaning vehicles for PES.
- Continue to proactively monitor call demand to ensure staffing levels are appropriate for 111.
- Continue to review call audit data to meet the required national targets for 111.
- Continue with plan of safeguarding training for all clinicians for 111.
Summary
It has been an extremely challenging 12 months for the NHS as a system, the North West and for NWAS. However, there are now definite signs of improvements and a reduction in delays for NWAS. It has been pleasing to see the innovative way NWAS has responded to many of the challenges faced that will continue during the coming years. Lead commissioners would like to thank NWAS and all their staff for the hard work undertaken during this extremely challenging period and the support they have given to the population of the North West, outlined well in this Quality Account.
Statement from Lancashire County Council Health Scrutiny Committee
The Lancashire County Council Health Scrutiny function welcomed the detail included in the Quality Accounts report on the examples of the challenges faced in 2022/23 and how improvements had been made.
The range of information that the trust is required to reference in this report was acknowledged, and members noted the challenges in producing a report for both professionals and the public. The Quality Account is well presented and reflects the requirements to benchmark against peers.
The Committee noted that due to the complexity of the information reported, consideration could be given to producing a summary document of the report with the focus on patients and the public as the key audience.
Members noted that there appeared to be little information on staffing and would like to have seen more detail on this area, the challenges and plans in place.
However, overall members felt that the report was well set out with a good balance of information and were particularly struck by the number of hours lost due to challenges with hospital handovers.
The trust should be commended in providing a very comprehensive report which was felt to be an honest reflection of the challenges faced.
The Lancashire Health Scrutiny function welcomed the opportunity to comment on the North West Ambulance Service NHS Trust Quality Accounts for 2022/23 and would welcome early involvement with the planning process to produce the trust’s 2023/24 Quality Account.
Appendix 1: Glossary of terms
AACE
The Association of Ambulance Chief Executives provides ambulance services with a central organisation that supports, coordinates, and implements nationally agreed policy.
Advanced Paramedics (APs)
Advanced paramedics offer a high level of clinical skills and leadership. They co-ordinate and provide clinical advice for some of the more complex incidents we attend, whilst also being responsible for a team of senior paramedics.
AED
Automated external defibrillators
ARP
Ambulance Response Programme: In 2017, following the largest clinical ambulance trials in the world, NHS England implemented new ambulance standards across the country. This was to ensure the sickest patients get the fastest response and that all patients get the right response first time.
BAF
Board assurance framework is used to record and report an organisational key strategic objectives, risks, controls and assurances to the board.
C1
Category 1: An immediate response to a life-threatening condition, such as cardiac or respiratory arrest. Response time to 90% of all incidents is 15 minutes.
C2
Category 2: A serious condition, such as stroke or chest pain, which may require rapid assessment and/or urgent transport. Response time to 90% of all incidents is 40 minutes.
C3
Category 3: An urgent problem, such as an uncomplicated diabetic issue, which requires treatment and transport to an acute setting. Response time to 90% of all incidents is 2 hours.
C4
Category 4: A non-urgent problem, such as stable clinical cases, which requires transportation to a hospital ward or clinic. Response time to 90% of all incidents is 3 hours.
Cardiac arrest
A medical condition wherein the heart stops beating effectively, requiring CPR and sometimes requiring defibrillation.
CCG
Clinical Commissioning Groups (CCGs) were created following the Health and Social Care Act in 2012 and replaced Primary Care Trusts on 1 April 2013. They are clinically led statutory NHS bodies responsible for the planning and commissioning of health care services for their local area.
CEO
Chief Executive Officer.
CHUB
The clinical hub is a department within the NWAS emergency operations centres that is made up of a multidisciplinary team including clinicians, dispatchers, navigators and managers.
Cleric
Ambulance software solution.
Community First Responder (CFR)
A member of the public who volunteers to provide an immediate response and first aid to patients requesting ambulance assistance.
Complementary Resources
Non ambulance trust providers of potentially life-saving care, e.g., CFRs St John Ambulance, Red Cross, Mountain Rescue, Air Ambulance.
CCA
Civil Contingencies Act, 2004 requires NHS organisations, and providers of NHS-funded care, to show that they can deal with a wide range of incidents and emergencies that could affect health or patient care while maintaining services.
CPR
Cardiopulmonary Resuscitation.
CQC
Care Quality Commission is the independent regulator of all health and social care services in England.
CQUIN
The Commissioning for Quality and Innovation (CQUIN) framework supports improvements in the quality of services and the creation of new, improved patterns of care.
Datix Cloud IQ
Datix Cloud IQ is a profound shift in focus for a healthcare risk management application, moving beyond the simple capture and review of data on adverse outcomes towards a managed process of exposing and resolving the issues that lead to those outcomes.
Defibrillator (also AED)
Medical equipment to provide an electric shock to a patient’s heart which is not functioning
properly.
DoS
The Directory of Services (DoS) is a central directory that is integrated with NHS Pathways and is automatically accessed if the patient does not require an ambulance or by any attending clinician in the urgent and emergency care services.
DSPT
The Data Security and Protection Toolkit is an online self-assessment tool that allows
organisations to measure their performance against the National Data Guardian’s 10 data security standards. All organisations that have access to NHS patient data and systems must use this toolkit to provide assurance that they are practising good data security and that personal information is handled correctly.
Duty of Candour
Every health and care professional must be open and honest with patients and people in their care when something that goes wrong with their treatment or care causes, or has the potential to cause, harm or distress.
ECG
Electrocardiogram (ECG) is a simple test that can be used to check a heart’s rhythm and electrical activity.
EOC
Emergency Operational Control receives and responds to 999 calls and other calls for ambulance service assistance.
EPR
Electronic Patient Record is a periodic health care record of a single individual, provided mainly by one healthcare organisation.
ERISS
ERISS is a web-based application, designed to enhance information sharing and collaborative working between the North West Ambulance Service (NWAS) and its key stakeholders. The system supports the transfer of referral information to external organisations in the North West and provides a secure portal for organisations to inform of care planning arrangements for specific patient groups.
EPRR
Emergency Preparedness, Resilience and Response is an NHS organisational plan for, and response to, a wide range of incidents and emergencies that could affect health or patient care. These could be anything from extreme weather conditions to an outbreak of an infectious disease or a major transport accident.
EDS
The Equality Delivery System (EDS) is a system that helps NHS organisations improve the services they provide for their local communities and provide better working environments, free of discrimination, for those who work in the NHS, while meeting the requirements of the Equality Act 2010.
FAST
A simple test for the presence of a stroke – Face, Arms, Speech, Time.
FFT
The NHS Friends and Family Test was created to help service providers and commissioners understand whether patients are happy with the service provided, or where improvements are needed. It is a quick and anonymous way to give your views after receiving NHS care or treatment.
FTSU
Freedom to speak up.
Gender Pay Gap Reporting
Organisations with 250 or more employees are mandated by the government to report annually on their gender pay gap. The requirements of the mandate within the Equality Act 2010 (Gender Pay Gap Information) Regulations 2017, are to publish information relating to pay for six specific measures as detailed in this report.
Green room Internal digital communication area for our staff.
HALO module
Hospital Arrival Screens (HAS) are used to show what time an ambulance arrives at hospital, what time a patient handover occurs and what time a vehicle is cleared to attend another job. Since October 2022, Hospital Arrival Screens have a new capability to capture when patient delays occur via the HALO module.
HSE
Health & Safety Executive is a regulatory body to ensure safe working practices are adhered to.
HSIB
Healthcare Safety Investigations Branch was formed in 2017 and are dedicated to improving patient safety through independent investigations into NHS-funded care across England.
HSIB is funded by the Department of Health and Social Care and currently hosted by NHS England.
ICS
Integrated care systems (ICSs) are partnerships between the organisations that meet health and care needs across an area, to coordinate services and to plan in a way that improves population health and reduces inequalities between different groups.
Integrated Care Board
Each Integrated Care System (ICS) will have an Integrated Care Board (ICB), a statutory organisation bringing the NHS together locally to improve population health and establish shared strategic priorities within the NHS. When ICBs are legally established, clinical commissioning groups (CCGs) will be abolished.
IPC
Infection Prevention and Control.
JRCALC
Joint Royal Colleges Ambulance Liaison Committees role is to provide robust clinical speciality advice to ambulance services within the UK and it publishes regularly updated clinical guidelines.
Just Culture
Just Culture is about creating a culture of fairness, openness and learning in the NHS. This is to make colleagues feel confident to speak up when things go wrong, rather than fearing blame. Supporting colleagues to be open about mistakes allows valuable lessons to be learnt.
LfD
Learning from deaths process sets out the practices used within our service to review and learn from the deaths of patients who had been under our care. The process is led by the Clinical Audit team and senior clinicians. This learning ensures we can protect future patients from avoidable harm, reduce unwarranted variation and provide truly patient- centred care.
LMS
Local Maternity Systems
MACA
Requests for Military Aid to the Civil Authorities (MACA) from the NHS in England.
MERIT
The Medical Emergency Response Incident Team (MERIT) forms an integral part of the NHS response to major, mass casualty and critical incidents, providing advanced medical advice at a range of emergency incidents.
NACQI/ACQI/AQI
National Ambulance Clinical Quality Indicator.
NEWS score
NEWS is a tool developed by the Royal College of Physicians which improves the detection and response to clinical deterioration in adult patients and is a key element of patient safety and improving patient outcomes.
NHSE
NHS England leads the National Health Service (NHS) in England.
NHS Pathways
NHS Pathways is a clinical tool used for assessing, triaging and directing the public to urgent and emergency care services.
NIHR Applied Research Collaborations
The National Institute for Health Research (NIHR) is the nation’s largest funder of health and care research and provides the people, facilities and technology that enables research to thrive. NIHR Applied Research Collaborations (ARCs) support applied health and care research that responds to, and meets, the needs of local populations and local health and care systems.
NIHR CRN
National Institute for Health Research Clinical Research Network (CRN) supports patients, the public and health and care organisations across England to participate in high-quality research, thereby advancing knowledge and improving care. The CRN is comprised of 15
Local Clinical Research Networks and 30 Specialties who coordinate and support the delivery of high-quality research both by geography and therapy area. National leadership and coordination are provided through the CRN Coordinating Centre.
NRLS
National Reporting and Learning System.
NWAS
North West Ambulance Service NHS Trust.
Ockenden report
The Ockenden report found a string of “repeated failures” spanning a period of 20 years – including at least 304 cases where there was avoidable harm. As a result of these failures, babies died or were left seriously disabled owing to catastrophic mistakes at the Shrewsbury and Telford Hospital NHS Trust.
Patient Safety Incident Reporting Framework
Patient Safety Incident Response Framework (PSIRF), outlines how providers should respond to patient safety incidents and how and when a patient safety investigation should be conducted.
Paramedic
A state registered ambulance healthcare professional.
PCN
Primary care networks are groups of practices working together to focus local patient care.
PDSA cycles
The Plan-Do-Study-Act cycle is shorthand for testing a change i.e., by planning it, trying it, observing the results, and acting on what is learned. This is the scientific method, used for action-oriented learning.
PDG
Patient Group Directions (PGDs) provide a legal framework that allows some registered health professionals to supply and/or administer specified medicines to a pre-defined group of patients, without them having to see a prescriber.
PES
Paramedic Emergency Service responds to 999 emergency ambulance calls.
Power BI
Power BI is a collection of software services, apps, and connectors that work together to turn your unrelated sources of data into coherent, visually immersive, and interactive insights.
PPE
Personal protective equipment protects the user against health or safety risks at work.
PPP
Trust’s Patient and Public Panel consists of volunteers who live in the North West of England and are involved in public and patient engagement activities e.g. Responding to surveys, giving feedback on publications, focus groups activities, attending committees or formal meetings.
PSED
Public Sector Equality Duty (PSED) is part of the Equality Act, came into force in April 2011. It requires NHS organisations to eliminate unlawful discrimination, advance equality of opportunity, and foster good relations.
PTS
Patient Transport Service – Non-emergency transport service that provides for hospital transfers, discharges and outpatients appointments for those patients unable to make their own travel arrangements.
PTS Bureau
The Patient Transport Service Bureau is the Patient Transport Service Controls and Contact Centre combined. The team not only provide access to PTS through the Contact Centre but manage all the activity through the control and planning functions and some of that is acting as broker using different types of third-party suppliers.
PTS CRU
The Patient Transport Service Central Rostering Unit undertake the rostering for the whole of the service line across the region and have responsibility for engagement regarding fleet and estates through their sector manager.
QAV
The purpose of QAVs is to provide assurance to the trust about the quality and safety of operational premises, vehicles and services at sector level and provide internal second line assurance and information in relation to key lines of enquiry from the Care Quality Commission.
QI
The term ‘quality improvement’ refers to the systematic use of methods and tools to try to continuously improve quality of care and outcomes for patients. There are a range of different methods and tools, such as Lean, Six Sigma and the Institute for Healthcare Improvement’s Model for Improvement.
RCF
Research capability funding.
RCQAC
Regional Clinical Quality Assurance Committee.
RIDDOR
Reporting of Injuries, Diseases and Dangerous Occurrences Regulations
ROSC
Return of Spontaneous Circulation.
ROSE
Review of serious events (ROSE) group oversees the reporting, actions and learning drawn from serious incidents.
SafeCheck
SafeCheck is an electronic database which was originally designed to replace paper process checks e.g., vehicle, equipment and medicine check book. SafeCheck is now being used captured routine audit work e.g., Infection Prevention and Control.
SDEC
Same day emergency care is one of the many ways the NHS is working to provide the right care, in the right place, at the right time for patients. It aims to benefit both patients and the healthcare system by reducing waiting times and hospital admissions, where appropriate.
Service Finder
Service finder enables clinicians to review where appropriate alternative services are available to refer patients to when A&E is not suitable. The regional Directory of Service (DOS) lead has developed ambulance referrals to ensure services most appropriate for our clinicians are highlighted quickly.
SharePoint
SharePoint is a digital platform that enables document sharing and news updates.
SJR
Structured judgement reviews are a methodology used for investigations.
SMART programme
Our internal digital and quality improvement programme.
SMS
Short messaging service- text messaging service component of most telephone, Internet, and mobile device systems.
SOP
Standard operating procedure is a set of step-by-step instructions to help teams carry out routine operations.
SPTLs
Senior paramedic team leader working as part of a crew or as a solo responder to attend urgent and critical emergency situations in a variety of environments. They use advanced clinical skills and manage a clinical team.
StEIS
Strategic Executive Information System.
STEMI
ST Elevation Myocardial Infarction – A life threatening heart attack.
Stroke
Blockage or bleeding of the blood vessels in the brain that can lead to death or disability.
UEC
Urgent and Emergency Care (UEC) services perform a critical role in keeping the population healthy.
Utstein
Cardiac arrest and CPR outcome reporting process.
VCSE
VCSE means an incorporated voluntary, community or social enterprise organisation which serves communities solely within England and which is either: (a) a charity, Community Interest Company or Community Benefit. Society, registered with the relevant registry body.
What3words
What3words is a fast and simple online interface that allows you to convert 3-word addresses to coordinates.
WDES
Workforce Disability Equality Standard is a set of ten specific measures (metrics) which enables NHS organisations to compare the workplace and career experiences of disabled and non-disabled staff.
WRES
Workforce Race Equality Standard requires NHS trusts to self-assess against nine indicators of workplace experience and opportunity. Four indicators relate specifically to workforce data, four are based on data from the national NHS staff survey questions, and one considers black minority ethnic representation on board.
Appendix 2: Contact details
If you have any questions or concerns after reading this report, please contact us: North West Ambulance Service NHS Trust
Headquarters Ladybridge Hall Chorley New Rd Bolton Lancashire
BL1 5DD
For general enquiries please use:
- Telephone: 01204 498400
- E-mail: [email protected]
For enquiries specific to the Quality Account, please contact Maxine Power, Executive Director of Quality, Innovation and Improvement on:
- Telephone: 01204 498400
- E-mail: [email protected]
Should you wish to access any of the trust publications mentioned in this Quality Account they can be accessed on the trust website at www.nwas.nhs.uk.